Breastfeeding Failure and Determinants: A Qualitative Study in Indonesia
Abstract
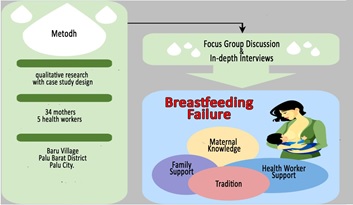
Exclusive breastfeeding has a significant impact on the growth and development of children. The low coverage of exclusive breastfeeding has significantly contributed to stunting in this country. This study aimed to describe the determinants of the failure of exclusive breastfeeding from the aspect of the mother's knowledge, breast problems, family support, support from health workers, and traditions. The research method was qualitative with a case study design. The sampling technique used purposive sampling with 34 mothers and five cadres. Data was collected using FGD (Focus Group Discussion) and In-depth Interviews. Data analysis using content analysis and data validation using triangulation techniques. The results showed that the dominant mother did not know about exclusive breastfeeding. Breast problems were the dominant determinant of the failure of exclusive breastfeeding. Families and health workers had not provided good social support to mothers. The tradition found was providing sugar water and rice water to infants aged less than 6 (six). This study found that maternal knowledge, breast problems, family support, support from health workers, and traditions were the determinants of the failure of exclusive breastfeeding. This study recommends the need for education for mothers, families, and health workers to understand the urgency of exclusive breastfeeding.
Downloads
References
Agho, K. E., Ezeh, O. K., Ghimire, P. R., Uchechukwu, O. L., Stevens, G. J., Tannous, W. K., & Maternal, G. (2019). Exclusive breastfeeding rates and associated factors in 13 “economic Community of West African States”(ECOWAS) countries. Nutrients, 11(12), 3007. https://doi.org/10.3390/nu11123007
Ahmed, K. Y., Page, A., Arora, A., & Ogbo, F. A. (2019). Trends and determinants of early initiation of breastfeeding and exclusive breastfeeding in Ethiopia from 2000 to 2016. International breastfeeding journal, 14(1), 1-14. https://doi.org/10.1186/s13006-019-0234-9
Ajami, M., Abdollahi, M., Salehi, F., Oldewage-Theron, W., & Jamshidi-Naeini, Y. (2018). The association between household socioeconomic status, breastfeeding, and infants' anthropometric indices. International journal of preventive medicine, 9. https://dx.doi.org/10.4103%2Fijpvm.IJPVM_52_17
Amir, L. H. (2014). Breastfeeding in public:“You can do it?”. International breastfeeding journal, 9(1), 1-3. https://doi.org/10.1186/s13006-014-0026-1
Angraresti, I. E., & Syauqy, A. (2016). Faktor-faktor yang berhubungan dengan kegagalan pemberian asi eksklusif di kabupaten semarang. Journal of Nutrition College, 5(4), 321-327. https://ejournal3.undip.ac.id/index.php/jnc/article/view/16431
Bartington, S., Griffiths, L. J., Tate, A. R., & Dezateux, C. (2006). Are breastfeeding rates higher among mothers delivering in Baby Friendly accredited maternity units in the UK?. International Journal of Epidemiology, 35(5), 1178-1186. https://doi.org/10.1093/ije/dyl155
Carolin, B. T., & Kholihah, K. (2019). Faktor-Faktor Yang Berhubungan Dengan Peranan Tenaga Kesehatan Terhadap Dukungan Pemberian Asi Eksklusif Di Rumah Sakit M Jakarta Selatan. Jurnal Akademi Keperawatan Husada Karya Jaya, 5(1). http://ejurnal.husadakaryajaya.ac.id/index.php/JAKHKJ/article/view/103
Dewi, P. D. P. K. (2020). Prediktor Kegagalan Pemberian ASI Eksklusif di Wilayah Kerja Puskesmas Sawan I Kabupaten Buleleng. Jurnal Ilmiah Bidan, 5(1). https://www.e-journal.ibi.or.id/index.php/jib/article/view/147
Dinas Kesehatan Kota Palu. (2021). Profil Kesehatan Kota Palu Tahun 2020. Palu. https://dinkes.palukota.go.id/program/profil_kesehatan
Francis, J., Mildon, A., Stewart, S., Underhill, B., Tarasuk, V., Di Ruggiero, E., & O'Connor, D. L. (2020). Vulnerable mothers' experiences breastfeeding with an enhanced community lactation support program. Maternal & child nutrition, 16(3), e12957. https://doi.org/10.1111/mcn.12957
Hamidah, N., & Kuntoro, K. (2016). Peran Karakteristik Responden dan Dukungan Tenaga Kesehatan dalam Identifikasi Faktor yang Terkait dengan Kegagalan Pemberian ASI Eksklusif. Jurnal Biometrika dan Kependudukan, 5(1), 52-60. https://doi.org/10.20473/jbk.v5i1.2016.52-60
Hamidah, S. (2018). Hubungan Antara Dukungan Keluarga Dengan Pemberian ASI Eksklusif Pada Bayi Usia 0-6 Bulan. Jurnal Midpro, 8(1), 9. https://doi.org/10.30736/midpro.v8i1.2
Horta, B. L., & de Lima, N. P. (2019). Breastfeeding and type 2 diabetes: systematic review and meta-analysis. Current Diabetes Reports, 19(1), 1-6. https://doi.org/10.1097/MCO.0000000000000453
Idawati, I., Mirdahni, R., Andriani, S., & Yuliana, Y. (2021). Analisis Penyebab Kegagalan Pemberian Asi Eksklusif pada Bayi di RSUD Tgk. Chik Ditiro Kabupaten Pidie. Sang Pencerah: Jurnal Ilmiah Universitas Muhammadiyah Buton, 7(4), 593-608. https://doi.org/10.35326/pencerah.v7i4.1573
Jatmika, S. E. D., Shaluhiyah, Z., & Suryoputro, A. (2016). Dukungan Tenaga Kesehatan Untuk Meningkatkan Niat Ibu Hamil Dalam Memberikan ASI Eksklusif di Wilayah Kerja Puskesmas Gondokusuman, Kota Yogyakarta. Jurnal Promosi Kesehatan Indonesia, 9(2), 196-205. https://ejournal.undip.ac.id/index.php/jpki/article/view/12734
Jedrychowski, W., Perera, F., Jankowski, J., Butscher, M., Mroz, E., Flak, E., & Sowa, A. (2012). Effect of exclusive breastfeeding on the development of children’s cognitive function in the Krakow prospective birth cohort study. European journal of pediatrics, 171(1), 151-158. https://doi.org/10.1007/s00431-011-1507-5
Kementerian Kesehatan RI. (2021). Profil Kesehatan Indonesia Tahun 2020. Jakarta. https://pusdatin.kemkes.go.id/resources/download/pusdatin/profil-kesehatan-indonesia/Profil-Kesehatan-Indonesia-Tahun-2020.pdf
Mannan, H. (2018). Early infant feeding of formula or solid foods and risk of childhood overweight or obesity in a socioeconomically disadvantaged region of Australia: a longitudinal cohort analysis. International journal of environmental research and public health, 15(8), 1685. https://doi.org/10.3390/ijerph15081685
Moss, B. G., & Yeaton, W. H. (2014). Early childhood healthy and obese weight status: potentially protective benefits of breastfeeding and delaying solid foods. Maternal and child health journal, 18(5), 1224-1232. https://doi.org/10.1007/s10995-013-1357-z
Negin, J., Coffman, J., Vizintin, P., & Raynes-Greenow, C. (2016). The influence of grandmothers on breastfeeding rates: a systematic review. BMC pregnancy and childbirth, 16(1), 1-10. https://doi.org/10.1186/s12884-016-0880-5
Notoatmodjo, S., 2014, Promosi Kesehatan dan Perilaku Kesehatan. Jakarta: Rineka Cipta.
Ogbo, F. A., Agho, K., Ogeleka, P., Woolfenden, S., Page, A., Eastwood, J., & Global Child Health Research Interest Group. (2017). Infant feeding practices and diarrhoea in sub-Saharan African countries with high diarrhoea mortality. PloS one, 12(2), e0171792. https://doi.org/10.1371/journal.pone.0171792
Ogbo, F. A., Dhami, M. V., Awosemo, A. O., Olusanya, B. O., Olusanya, J., Osuagwu, U. L., & Agho, K. E. (2019). Regional prevalence and determinants of exclusive breastfeeding in India. International breastfeeding journal, 14(1), 1-12. https://doi.org/10.1186/s13006-019-0214-0
Ogbo, F. A., Page, A., Idoko, J., Claudio, F., & Agho, K. E. (2016). Diarrhoea and suboptimal feeding practices in Nigeria: evidence from the national household surveys. Paediatric and perinatal epidemiology, 30(4), 346-355. https://doi.org/10.1111/ppe.12293
Pattison, K. L., Kraschnewski, J. L., Lehman, E., Savage, J. S., Downs, D. S., Leonard, K. S., & Kjerulff, K. H. (2019). Breastfeeding initiation and duration and child health outcomes in the first baby study. Preventive medicine, 118, 1-6. https://doi.org/10.1016/j.ypmed.2018.09.020
Ramadani, M. (2017). Dukungan keluarga sebagai faktor dominan keberhasilan menyusui eksklusif. Media Kesehatan Masyarakat Indonesia, 13(1), 34-41. https://journal.unhas.ac.id/index.php/mkmi/article/view/1580
Scott, J. A., Kwok, Y. Y., Synnott, K., Bogue, J., Amarri, S., Norin, E., & INFABIO Project Team. (2015). A comparison of maternal attitudes to breastfeeding in public and the association with breastfeeding duration in four European countries: results of a cohort study. Birth, 42(1), 78-85. https://doi.org/10.1111/birt.12138
Setyaningsih, F. T. E., & Farapti, F. (2019). Hubungan Kepercayaan dan Tradisi Keluarga pada Ibu Menyusui dengan Pemberian ASI Eksklusif di Kelurahan Sidotopo, Semampir, Jawa Timur. Jurnal Biometrika Dan Kependudukan, 7(2), 160–167. https://doi.org/10.20473/jbk.v7i2.2018.160-167
Solo, K. M. B., & Novita, R. V. T. (2020). Status Breast condition and Babies Health Influence Practice of Exclusive Breastfeeding. Media Keperawatan Indonesia, 3(3), 144. https://doi.org/10.26714/mki.3.3.2020.144-149
Syeda, B., Agho, K., Wilson, L., Maheshwari, G. K., & Raza, M. Q. (2021). Relationship between breastfeeding duration and undernutrition conditions among children aged 0–3 Years in Pakistan. International Journal of Pediatrics and Adolescent Medicine, 8(1), 10-17. https://doi.org/10.1016/j.ijpam.2020.01.006
Victora, C. G., Bahl, R., Barros, A. J., França, G. V., Horton, S., Krasevec, J., & Group, T. L. B. S. (2016). Breastfeeding in the 21st century: epidemiology, mechanisms, and lifelong effect. The lancet, 387(10017), 475-490. https://doi.org/10.1016/S0140-6736(15)01024-7
Victora, C. G., Horta, B. L., De Mola, C. L., Quevedo, L., Pinheiro, R. T., Gigante, D. P., & Barros, F. C. (2015). Association between breastfeeding and intelligence, educational attainment, and income at 30 years of age: a prospective birth cohort study from Brazil. The lancet global health, 3(4), e199-e205. https://doi.org/10.1016/S2214-109X(15)70002-1
World Health Organization. (2016). Infant and young child feeding. http://www.who.int/mediacentre/factsheets/fs342/en/
World Health Organization. (2019a). Global Breastfeeding Scorecard, 2019: Increasing Commitment to Breastfeeding through Funding and Improved Policies and Programmes. Geneva, Switzerland. https://apps.who.int/iris/handle/10665/326049
World Health Organization. (2019b). Global Targets 2025. To Improve Maternal, Infant and Young Child Nutrition. https://www.who.int/multi-media/details/Nutrition-global-targets-2025
Yanuarini, T. A., Rahayu, D. E., & Prahitasari, E. (2017). Hubungan pengetahuan dengan sikap ibu dalam pemberian ASI eksklusif di wilayah kerja puskesmas pranggang kabupaten kediri. Jurnal Ilmu Kesehatan, 3(1), 1-9. https://doi.org/10.32831/jik.v3i1.39
Copyright (c) 2022 Rasyika Nurul Fadjriah, Shendy Krishnasari, Shendy Krishnasari

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
Authors retain copyright and grant the journal right of first publication with the work simultaneously licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License that allows others to share the work with an acknowledgment of the work's authorship and initial publication in this journal.
Authors are able to enter into separate, additional contractual arrangements for the non-exclusive distribution of the journal's published version of the work (e.g., post it to an institutional repository or publish it in a book), with an acknowledgment of its initial publication in this journal.
Authors are permitted to publish their work online in third parties as it can lead to wider dissemination of the work.




