Maternal Anaemia and Low Birth Weight in Gowa District, Indonesia
Abstract
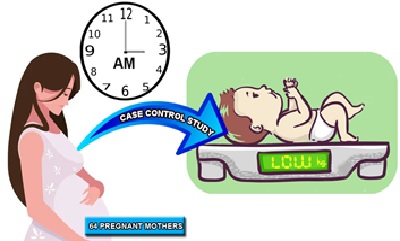
Low Birth Weight (LBW) is the main cause of the high infant mortality rate, especially in the perinatal period. LBW is extremely susceptible to infection, a very big risk of experiencing problems when the baby grows up to adulthood. This study aimed to determine the association between high-risk expectant mother (mother's age, gestational age, maternal anemia, maternal nutritional status, and family socioeconomic status) with LBW. This research was a quantitative research with an observational analytic approach with a case control study design. The population in this study were all mothers who gave birth to babies in the working area of Somba Opu Health Center in 2020-2021. The sample in this study were 64 expectant mothers consisting of 32 cases and 32 controls taken by using a purposive sampling technique with the inclusion criteria of expectant mothers domiciled in Somba Opu sub-district having completed examination records. The association analysis used Chi Square test with 95% confidence interval. The results showed that there was a significant association between maternal anemia with LBW (p=0,003, OR=7) and there is no association between maternal age (p=0,305, OR=1,9), gestational distance (p=0,426, OR=2,8), maternal nutritional status (p=0,197, OR=2,3), and socioeconomic status of the family (p=0,238, OR=2,5) with LBW in the working area of Somba Opu Health Center, Gowa Regency in 2021. The researcher recommends that the expectant mothers routinely perform ANC in order to increase early detection of high-risk expectant mothers, and increase maternal nutritional intake by consuming balanced nutrition, taking Fe tablets, doing PMT for expectant mothers which can increase maternal Hb levels.
Downloads
References
Al-Maraghi, A. M. (1946). Tafsir Al Maraghi. Lebanon: Darul al-Kutub Beirut
Anggraeni, D., Utomo, B., & Suryawan, A. (2014). Risk Factors Of Low Birth Weight (Lbw) Incidence. A Case Control Study. Folia Medica Indonesiana, 50(4). https://journal.unair.ac.id/download-fullpapers-fmi90872afb19full.pdf
Ash-Shiddieqy, M. H. (2013). Falsafah Hukum Islam. Pustaka Rizki Putra
As-Subki, A. Y. (2010). Fiqh Keluarga : Pedoman Berkeluarga Dalam Islam. Jakarta : Amzah
Badan Pusat Statistik Provinsi Sulawesi Selatan. (2015). Jumlah Bayi Lahir, Bayi Berat Badan Lahir Rendah (BBLR), BBLR Dirujuk, Dan Bergizi Buruk Menurut Kabupaten/Kota Di Provinsi Sulawesi Selatan, 2015. https://sulsel.bps.go.id/dynamictable/2016/08/15/292/jumlah-bayi-lahir-bayi-berat-badan-lahir-rendah-bblr-bblr-dirujuk-dan-bergizi-buruk-menurut-kabupaten-kota-di-provinsi-sulawesi-selatan-2015.html
Bird, A. L., Grant, C. C., Bandara, D. K., Mohal, J., Atatoa‐Carr, P. E., Wise, M. R., & Morton, S. M. (2017). Maternal health in pregnancy and associations with adverse birth outcomes: evidence from growing up in New Zealand. Australian and New Zealand Journal of Obstetrics and Gynaecology, 57(1), 16-24. https://doi.org/10.1111/ajo.12557
Brannon, P. M., & Taylor, C. L. (2017). Iron supplementation during pregnancy and infancy: uncertainties and implications for research and policy. Nutrients, 9(12), 1327. https://doi.org/10.3390/nu9121327
Correa-de-Araujo, R., & Yoon, S. S. (2021). Clinical outcomes in high-risk pregnancies due to advanced maternal age. Journal of Women's Health, 30(2), 160-167. https://doi.org/10.1089/jwh.2020.8860
Demelash, H., Motbainor, A., Nigatu, D., Gashaw, K., & Melese, A. (2015). Risk factors for low birth weight in Bale zone hospitals, South-East Ethiopia: a case–control study. BMC pregnancy and childbirth, 15(1), 1-10. https://doi.org/10.1186/s12884-015-0677-y
Girma, S., Fikadu, T., Agdew, E., Haftu, D., Gedamu, G., Dewana, Z., & Getachew, B. (2019). Factors associated with low birthweight among newborns delivered at public health facilities of Nekemte town, West Ethiopia: a case control study. BMC pregnancy and childbirth, 19(1), 1-6. https://doi.org/10.1186/s12884-019-2372-x
Hadiwijaya, E., & Kumala, A. (2019). Hubungan kehamilan usia remaja dengan kejadian bayi berat lahir rendah (BBLR) di RSUD Ciawi-Kabupaten Bogor periode 2016-2017. Tarumanagara Medical Journal, 1(2), 270-276. https://journal.untar.ac.id/index.php/tmj/article/view/3850
Härkönen, J., Lindberg, M., Karlsson, L., Karlsson, H., & Scheinin, N. M. (2018). Education is the strongest socio‐economic predictor of smoking in pregnancy. Addiction, 113(6), 1117-1126. https://doi.org/10.1111/add.14158
Harvey, E. M., Strobino, D., Sherrod, L., Webb, M. C., Anderson, C., White, J. A., & Atlas, R. (2017). Community-academic partnership to investigate low birth weight deliveries and improve maternal and infant outcomes at a Baltimore city hospital. Maternal and child health journal, 21(2), 260-266. https://doi.org/10.1007/s10995-016-2153-3
Haryanti, S. Y., Pangestuti, D. R., & Kartini, A. (2019). Anemia dan kek pada ibu hamil sebagai faktor risiko kejadian bayi berat lahir rendah (BBLR)(studi di wilayah kerja puskesmas Juwana Kabupaten pati). Jurnal Kesehatan Masyarakat (Undip), 7(1), 322-329. https://ejournal3.undip.ac.id/index.php/jkm/article/view/22978
Hasriyani, H., Hadisaputro, S., Budhi, K., Setiawati, M., & Setyawan, H. (2018). Berbagai Faktor Risiko Kejadian Bayi Berat Lahir Rendah (BBLR)(Studi di Beberapa Puskesmas Kota Makassar). Jurnal Epidemiologi Kesehatan Komunitas, 3(2), 91-101. https://doi.org/10.14710/jekk.v3i2.4027
Howlader, S. U., Hossain, S., Juliana, F. M., & Asaduzzaman, M. (2018). Relationship among Maternal Height, Pre-Pregnancy Nutritional Status and Birth Weight of Neonates in Dhaka City. J Nutr Health Food Eng, 8(2), 00257. https://doi.org/10.15406/jnhfe.2018.08.00257
Intang, S. N. (2020). Hubungan Antara Umur Ibu Dan Paritas Tentang Kejadian Bayi Berat Lahir Rendah (BBLR) Di Rumah Sakit Umum Daerah Batara Siang Pangkep. Celebes Health Journal, 2(1), 24-32. http://journal.lldikti9.id/CPHJ/article/view/331
Jayanti, F. A., Dharmawan, Y., & Aruben, R. (2017). Faktor-faktor yang berhubungan dengan kejadian berat badan lahir rendah di wilayah kerja puskesmas bangetayu kota Semarang tahun 2016. Jurnal Kesehatan Masyarakat (Undip), 5(4), 812-822. https://ejournal3.undip.ac.id/index.php/jkm/article/view/18782
Kaur, S., Ng, C. M., Badon, S. E., Jalil, R. A., Maykanathan, D., Yim, H. S., & Mohamed, H. J. J. (2019). Risk factors for low birth weight among rural and urban Malaysian women. BMC Public Health, 19(4), 1-10. https://doi.org/10.1186/s12889-019-6864-4
Kementerian Kesehatan RI. (2019). Hasil Utama Riset Kesehatan Dasar 2018. https://www.litbang.kemkes.go.id/hasil-utama-riskesdas-2018/
Kementerian Perencanaan Pembangunan Nasional. 2020. Pilar Pembangunan Sosial. https://sdgs.bappenas.go.id/wp-content/uploads/2020/10/Metadata-Pilar-Sosial-Edisi-II.pdf
Kuchenbecker, J., Jordan, I., Reinbott, A., Herrmann, J., Jeremias, T., Kennedy, G., & Krawinkel, M. B. (2015). Exclusive breastfeeding and its effect on growth of Malawian infants: results from a cross-sectional study. Paediatrics and international child health, 35(1), 14-23. https://doi.org/10.1179/2046905514Y.0000000134
Kurnia, W., Hadju, V., & Muis, M. (2018). Hubungan Aktivitas Fisik Pada Ibu Hamil Dengan Berat Badan Lahir Di Kabupaten Jeneponto. Jurnal Kesehatan Masyarakat Maritim, 1(1). https://doi.org/10.30597/jkmm.v1i1.8701
Lawani, L. O., Iyoke, C. A., Onoh, R. C., Nkwo, P. O., Ibrahim, I. A., Ekwedigwe, K. C., & Ekine, A. A. (2016). Obstetric benefits of health insurance: A comparative analysis of obstetric indices and outcome of enrollees and non-enrollees in southeast Nigeria. Journal of Obstetrics and Gynaecology, 36(7), 946-949. https://doi.org/10.1080/01443615.2016.1174830
Liauw, J., Jacobsen, G. W., Larose, T. L., & Hutcheon, J. A. (2019). Short interpregnancy interval and poor fetal growth: Evaluating the role of pregnancy intention. Paediatric and perinatal epidemiology, 33(1), 073-085. https://doi.org/10.1111/ppe.12506
Owa, K. (2019). Chronic Energy Deficiency, Anemia as a Risk Factor for Low Birth Weight Babies in East Nusa Tenggara. Jurnal Kesehatan Primer, 4(1), 13-22. http://jurnal.poltekeskupang.ac.id/index.php/jkp/article/view/264
Permana, P., & Wijaya, G. B. R. (2019). Analisis faktor risiko bayi Berat Badan Lahir Rendah (BBLR) di Unit Pelayanan Terpadu (UPT) Kesehatan Masyarakat (Kesmas) Gianyar I tahun 2016-2017. Intisari Sains Medis, 10(3), 674-8. https://dx.doi.org/10.15562/ism.v10i3.481
Puskesmas Somba Opu. (2021). Rekapitulasi Laporan PWS-KIA Puskesmas Somba Opu Tahun 2020. Kabupaten Gowa.
Setiawan, I. (2017). Tafsir Ayat Al-Qur’an Tema Keperawatan, Kebidanan dan Fakta Ilmiahnya. Journal of Health Studies, 1(2), 197-212. http://dx.doi.org/10.31101/jhes.339
Shihab, M. Q. (2002). Tafsir Al-Mishbah Pesan, Kesan, dan Keserasian Al-Qur’an. Lentera Hati.
Stangret, A., Wnuk, A., Szewczyk, G., Pyzlak, M., & Szukiewicz, D. (2017). Maternal hemoglobin concentration and hematocrit values may affect fetus development by influencing placental angiogenesis. The Journal of Maternal-Fetal & Neonatal Medicine, 30(2), 199-204. https://doi.org/10.3109/14767058.2016.1168395
Sui, Y., Ahuru, R. R., Huang, K., Anser, M. K., & Osabohien, R. (2021). Household Socioeconomic Status and Antenatal Care Utilization Among Women in the Reproductive-Age. Frontiers in Public Health, 9. https://dx.doi.org/10.3389%2Ffpubh.2021.724337
Sujianti, S. (2018). Hubungan Usia Ibu dengan Kejadian Bayi Berat Lahir Rendah (BBLR) di Rsud Cilacap. Jurnal Kesehatan Al-Irsyad, 62-67. http://jka.stikesalirsyadclp.ac.id/index.php/jka/article/view/98
Sukmawati, S., Hendrayati, H., Chaerunnimah, C., & Nurhumaira, N. (2018). Status gizi ibu saat hamil, berat badan lahir bayi dengan stunting pada balita usia 06-36 bulan di Puskesmas Bontoa. Media Gizi Pangan, 25(1), 18-24. https://dx.doi.org/10.32382/mgp.v25i1.55
Syaikh, A. A. M. 2015. Tafsir Ibnu Katsir (Lubaabut Tafsiir Min Ibni Katsiir). 8th ed. Jakarta: Pustaka Imam asy-Syafi’i.
Tshotetsi, L., Dzikiti, L., Hajison, P., & Feresu, S. (2019). Maternal factors contributing to low birth weight deliveries in Tshwane District, South Africa. PloS one, 14(3), e0213058. https://doi.org/10.1371/journal.pone.0213058
World Health Organization. (2014). WHA Global Nutrition Targets 2025: Low Birth Weight Policy Brief. https://apps.who.int/iris/bitstream/handle/10665/149020/WHO_NMH_NHD_14.5_eng.pdf?ua=1
World Health Organization. (2015). The Global Prevalence of Anaemia in 2011. World Health Organization: Geneva, Switzerland
World Health Organization. (2019). “Newborns: Reducing Mortality. https://www.who.int/news-room/fact-sheets/detail/newborns-reducing-mortality
Copyright (c) 2022 Siti Latifah Burhan, Emmi Bujawati, Syarfaini Syarfaini, Andi Syamsiah Adha

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
Authors retain copyright and grant the journal right of first publication with the work simultaneously licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License that allows others to share the work with an acknowledgment of the work's authorship and initial publication in this journal.
Authors are able to enter into separate, additional contractual arrangements for the non-exclusive distribution of the journal's published version of the work (e.g., post it to an institutional repository or publish it in a book), with an acknowledgment of its initial publication in this journal.
Authors are permitted to publish their work online in third parties as it can lead to wider dissemination of the work.




