Exploring the Link Between Food Security, Health Services, and Family Income on Wasting Incidence Among Toddlers (0-59 Months)
Abstract
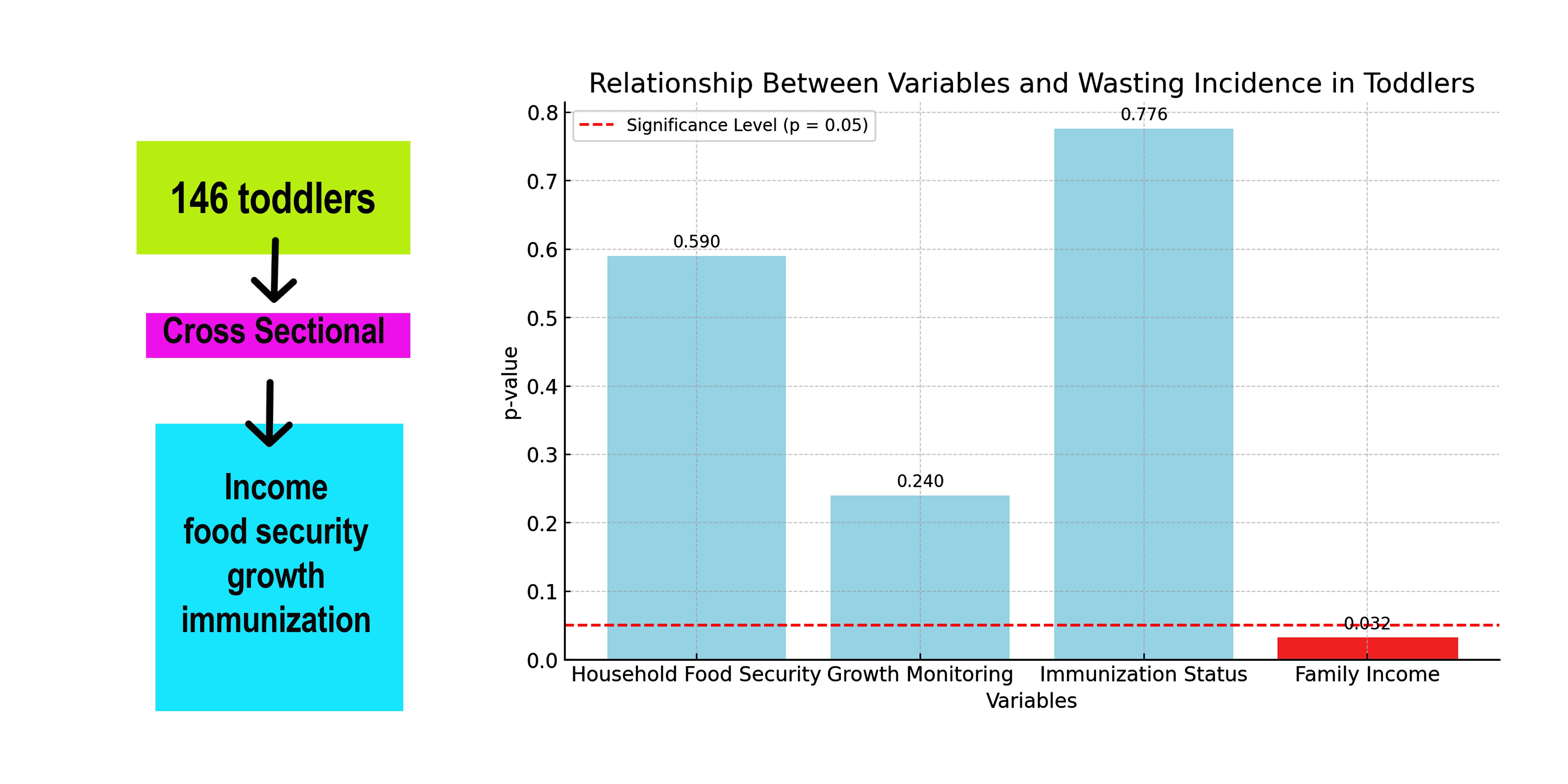
Wasting remains a significant nutritional challenge in Indonesia. Despite a reduction in its prevalence from 10.2% in 2018 to 7.1% in 2021, the rate still falls short of the national target of 7%. This study aims to examine the relationship between health services and family income on the incidence of wasting in toddlers aged 0-59 months in the Polombangkeng Utara sub-district, Takalar district. The research employed a quantitative approach with a cross-sectional study design. The population in this study consisted of toddlers aged 0-59 months in the North Polombangkeng sub-district, with a sample size of 146 toddlers. A probability sampling technique was used. The analysis was conducted using the chi-square test. The results of the chi-square test show that household food security is not related to the incidence of wasting, with a p-value of 0.590 (>0.05). Similarly, there is no relationship between growth monitoring and the incidence of wasting, with a p-value of 0.240 (>0.05), and no relationship between the completeness of immunization status and the incidence of wasting, with a p-value of 0.776 (>0.05). However, family income does show a relationship to the incidence of wasting, with a p-value of 0.032 (<0.05). This study indicates that food security and health services do not impact the incidence of wasting. In contrast, family income, which is a primary factor in nutritional problems, does have an impact on the incidence of wasting. The issue of wasting in toddlers can be prevented and addressed through specific and sensitive nutrition interventions.
Downloads
References
Abdurahman, A. A., Mirzaei, K., Dorosty, A. R., Rahimiforoushani, A., & Kedir, H. (2016). Household Food Insecurity May Predict Underweight and Wasting among Children Aged 24-59 Months. Ecology of Food and Nutrition, 55(5), 456-472. https://doi.org/10.1080/03670244.2016.1207069
Ahmed, M., Hokororo, A., Kidenya, B., Kabyemera, R., & Kamugisha, E. (2016). Prevalence of undernutrition and risk factors of severe undernutrition among children admitted to bugando medical centre in mwanza, tanzania. BMC Nutrition, 2(1). https://doi.org/10.1186/s40795-016-0090-6
Bawankule, R., Singh, A., Kumar, K., & Shetye, S. (2017). Does measles vaccination reduce the risk of acute respiratory infection (ari) and diarrhea in children: a multi-country study?. Plos One, 12(1), e0169713. https://doi.org/10.1371/journal.pone.0169713
Bekele, S., Fekadu, G., & Achamyeleh, A. (2021). Prevalence and factors associated with acute malnutrition among children in kamashi district, benishangul gumuz region, western ethiopia, 2019.. https://doi.org/10.21203/rs.3.rs-134719/v1
Bukari, M., Abubakari, M., Majeed, M., Abizari, A., Wemakor, A., & Atosona, A. (2019). Effect of maternal growth monitoring knowledge on stunting, wasting and underweight among children 0-18 months in tamale metropolis of ghana.. https://doi.org/10.21203/rs.2.16457/v1
Bukit, D., Keloko, A., & Ashar, T. (2021). Father's support and mother's behavior in stunting prevention efforts. Journal of Health Science and Prevention, 5(2), 100-105. https://doi.org/10.29080/jhsp.v5i2.521
Buzhardt, J., Leonard, J., Ai, J., Higgins, S., Greenwood, C., Consolver, K., & Carta, J. (2022). Technology to facilitate progress monitoring of infant–toddler growth and development: measuring implementation in community-based agencies. Journal of Special Education Technology, 38(2), 198-212. https://doi.org/10.1177/01626434221108882
Cunningham, K., Ruel, M., Ferguson, E., & Uauy, R. (2014). Women's empowerment and child nutritional status in south asia: a synthesis of the literature. Maternal and Child Nutrition, 11(1), 1-19. https://doi.org/10.1111/mcn.12125
Ernawati, R., Rahman, F., M, S., F, D., Sulistiawan, J., & Moslehpour, M. (2021). The effectiveness of web-based audio-visual media applications in monitoring children’s growth to prevent stunting. Advances in Decision Sciences, 25(3), 46-57. https://doi.org/10.47654/v25y2021i3p46-57
Gimaiyo, G., McManus, J., Yarri, M., Singh, S., Trevett, A., Moloney, G., & Lehmann, L. (2019). Can child-focused sanitation and nutrition programming improve health practices and outcomes? evidence from a randomised controlled trial in kitui county, kenya. BMJ Global Health, 4(1), e000973. https://doi.org/10.1136/bmjgh-2018-000973
Haq, I., He, X., Mujahid, A., Ibrahim, H., Mehmood, Z., Shah, J., & Miao, J. (2022). Preparedness to combat determinants of underweight-based child malnutrition in flood-affected areas of pakistan. Biomed Research International, 2022, 1-10. https://doi.org/10.1155/2022/6464901
Hidayat, S. I., Ardhany, Y. H., & Nurhadi, E. (2020). Assessment of Food Waste to Support Food Security. Agriekonomika, 9(2), 171-182. https://doi.org/10.21107/agriekonomika.v9i2.8787
Husnah, R. (2021). The relationship between family income, maternal knowledge and diet with the undernutrition status of children aged 6-24 months in the ditch health center area of West Pasaman Regency. Initium Medica Journal, 1(2), 1-7.
Indonesian Ministry of Health. (2019). Basic Health Research Results 2018. Ministry of Health, 53(9), 1689-1699.
Islam, R., Rahman, S., Rahman, M., Nomura, S., Silva, A., Lanerolle, P., & Rahman, M. (2019). Reducing childhood malnutrition in bangladesh: the importance of addressing socio-economic inequalities. Public Health Nutrition, 23(1), 72-82. https://doi.org/10.1017/s136898001900140x
Jayatissa, R., Herath, H. P., Perera, A. G., Dayaratne, T. T., De Alwis, N. D., & Nanayakkara, H.P. L. K. (2021). Impact of COVID-19 on child malnutrition, obesity in women and household food insecurity in underserved urban settlements in Sri Lanka: A prospective follow-up study. Public Health Nutrition, 24(11), 3233-3241. https://doi.org/10.1017/S1368980021001841
Jones, K., Thitiri, J., Ngari, M., & Berkley, J. (2014). Childhood malnutrition: toward an understanding of infections, inflammation, and antimicrobials. Food and Nutrition Bulletin, 35(2_suppl1), S64-S70. https://doi.org/10.1177/15648265140352s110
Khan, S., Zaheer, S., & Safdar, N. (2019). Determinants of stunting, underweight and wasting among children < 5 years of age: evidence from 2012-2013 pakistan demographic and health survey. BMC Public Health, 19(1). https://doi.org/10.1186/s12889-019-6688-2
Kien, V., Lee, H., Nam, Y., Oh, J., Giang, K., & Minh, H. (2016). Trends in socioeconomic inequalities in child malnutrition in vietnam: findings from the multiple indicator cluster surveys, 2000–2011. Global Health Action, 9(1), 29263. https://doi.org/10.3402/gha.v9.29263
Manzoni, G., Laillou, A., Chea, S., Hong, R., Wieringa, F., Berger, J., & Checchi, F. (2019). Child-sensitive wash composite score and the nutritional status in cambodian children. Nutrients, 11(9), 2142. https://doi.org/10.3390/nu11092142
Masthalina, H., Santosa, H., Sudaryat, E., & Zuska, F. (2021). Household food insecurity, level of nutritional adequacy, and nutritional status of toddlers in the coastal area of central tapanuli regency. Open Access Macedonian Journal of Medical Sciences, 9(E), 1371-1375. https://doi.org/10.3889/oamjms.2021.7571
Maulizar, R. (2023). The relationship between behavior, maternal education and the prevalence of wasting among toddlers in meureubo and kaway xvi districts, west aceh regency. Asian Journal of Advanced Research and Reports, 17(12), 108-115. https://doi.org/10.9734/ajarr/2023/v17i12590
Nepali, S., Simkhada, P., & Davies, I. (2020). Association between wasting and food insecurity among children under five years: findings from nepal demographic health survey 2016. BMC Public Health, 20(1). https://doi.org/10.1186/s12889-020-09146-x
Nguyen, C., & Nguyen, M. (2020). The roles of social economic status and undernutrition in regional disparities of the under‐five mortality rate in vietnam. Tropical Medicine & International Health, 25(11), 1362-1372. https://doi.org/10.1111/tmi.13475
Nwankwo, B., Mohammadnezhad, M., Hagan, V., Garatsa, C., & Barasa, E. (2022). Prevalence and determinants of undernutrition among under-five children in nigeria: a systematic review. Global Journal of Health Science, 14(11), 1. https://doi.org/10.5539/gjhs.v14n11p1
Ogbu, T., Scales, S., Almeida, M., Loenhout, J., Speybroeck, N., & Guha-Sapir, D. (2022). Predictors of exceeding emergency under-five mortality thresholds using small-scale survey data from humanitarian settings (1999 – 2020): considerations for measles vaccination, malnutrition, and displacement status. Archives of Public Health, 80(1). https://doi.org/10.1186/s13690-022-00916-0
Onís, M., Borghi, E., Arimond, M., Webb, P., Croft, T., Saha, K., & Flores‐Ayala, R. (2018). Prevalence thresholds for wasting, overweight and stunting in children under 5 years. Public Health Nutrition, 22(1), 175-179. https://doi.org/10.1017/s1368980018002434
Prendergast, A. (2015). Malnutrition and vaccination in developing countries. Philosophical Transactions of the Royal Society B Biological Sciences, 370(1671), 20140141. https://doi.org/10.1098/rstb.2014.0141
Rahmad, A., Iskandar, I., Fadjri, T., & Hadi, A. (2022). Utilization of the growth chart module in increasing mother's knowledge to monitor the grow up of toddlers. Kesmas Indonesia, 14(1), 110. https://doi.org/10.20884/1.ki.2022.14.1.640
Rahmad, A., Miko, A., Labatjo, R., Fajriansyah, F., Fitri, Y., & Suryana, S. (2020). Malnutrition prevalence among toddlers based on family characteristics: a cross-sectional study in the rural and urban areas of aceh, indonesia. Sri Lanka Journal of Child Health, 49(3), 263. https://doi.org/10.4038/sljch.v49i3.9145
Ramli, R., Sattu, M., Ismail, A., Lalusu, E., Lanyumba, F., Balebu, D., & Yani, A. (2022). Factors influencing the incidence of stunting in jaya bakti village, pagimana district, banggai regency. Open Access Macedonian Journal of Medical Sciences, 10(E), 303-307. https://doi.org/10.3889/oamjms.2022.8227
Rytter, M., Kolte, L., Briend, A., Friis, H., & Christensen, V. (2014). The immune system in children with malnutrition—a systematic review. Plos One, 9(8), e105017. https://doi.org/10.1371/journal.pone.0105017
Sahiledengle, B. (2024). Childhood undernutrition mediates the relationship between open defecation with anemia among ethiopian children: a nationally representative cross-sectional study. BMC Public Health, 24(1). https://doi.org/10.1186/s12889-024-18931-x
Sahiledengle, B., Petrucka, P., Kumie, A., Mwanri, L., Beressa, G., Atlaw, D., & Agho, K. (2022). Association between water, sanitation and hygiene (wash) and child undernutrition in ethiopia: a hierarchical approach. BMC Public Health, 22(1). https://doi.org/10.1186/s12889-022-14309-z
Setyani, L. and Anwar, K . (2022). The association between feeding practices and history of diarrhea with nutritional status of toddlers. Indonesian Journal of Public Health Nutrition, 3(1). https://doi.org/10.7454/ijphn.v3i1.6171
Simanjuntak, B., Haya, M., Suryani, D., Khomsan, A., & Ahmad, C. (2019). Maternal knowledge, attitude, and practices about traditional food feeding with stunting and wasting of toddlers in farmer families. Kesmas National Public Health Journal, 14(2). https://doi.org/10.21109/kesmas.v14i2.2712
Simbolon, D., Suryani, D., & Yorita, E. (2019). Prediction model and scoring system in prevention and control of stunting problems in under five-year-olds in indonesia. Jurnal Kesehatan Masyarakat, 15(2), 160-170. https://doi.org/10.15294/kemas.v15i2.13415
South Sulawesi Provincial Health Office. (2020). South Sulawesi Health Profile in 2019.
Susanti, A., Rinawan, F., & Amelia, I. (2019). Mothers knowledge and perception of toddler growth monitoring using iposyandu application. Global Medical & Health Communication (Gmhc), 7(2). https://doi.org/10.29313/gmhc.v7i2.3892
Syarif, I. (2024). The relationship between family food security and the nutritional status of toddlers in tamalate sub-district, makassar city. Jurnal Penelitian Pendidikan Ipa, 10(5), 2642-2647. https://doi.org/10.29303/jppipa.v10i5.6184
Tadesse, S. E., Mekonnen, T. C., Feleke, Y. W., Mesfine, M. A., Bekele, N. C., & Ali, H. (2020). Correlation between Agricultural Biodiversity, Dietary Diversity, Household Food Security and Associated Factors of Wasting among 6-59 Months old Children in Ambassel Woreda, North East Ethiopia. 1-14. https://doi.org/10.21203/rs.2.22888/v1
Wendt, A., Sparling, T., Waid, J., Mueller, A., & Gabrysch, S. (2019). Food and agricultural approaches to reducing malnutrition (faarm): protocol for a cluster-randomised controlled trial to evaluate the impact of a homestead food production programme on undernutrition in rural bangladesh. BMJ Open, 9(7), e031037. https://doi.org/10.1136/bmjopen-2019-031037
Copyright (c) 2024 Syamsul Alam, Iriyanti Harun, Rezki Nurfatmi

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
Authors retain copyright and grant the journal right of first publication with the work simultaneously licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License that allows others to share the work with an acknowledgment of the work's authorship and initial publication in this journal.
Authors are able to enter into separate, additional contractual arrangements for the non-exclusive distribution of the journal's published version of the work (e.g., post it to an institutional repository or publish it in a book), with an acknowledgment of its initial publication in this journal.
Authors are permitted to publish their work online in third parties as it can lead to wider dissemination of the work.