Portrait of Metabolic Syndrome by Gender in A Rural Area of Gowa Regency
Abstract
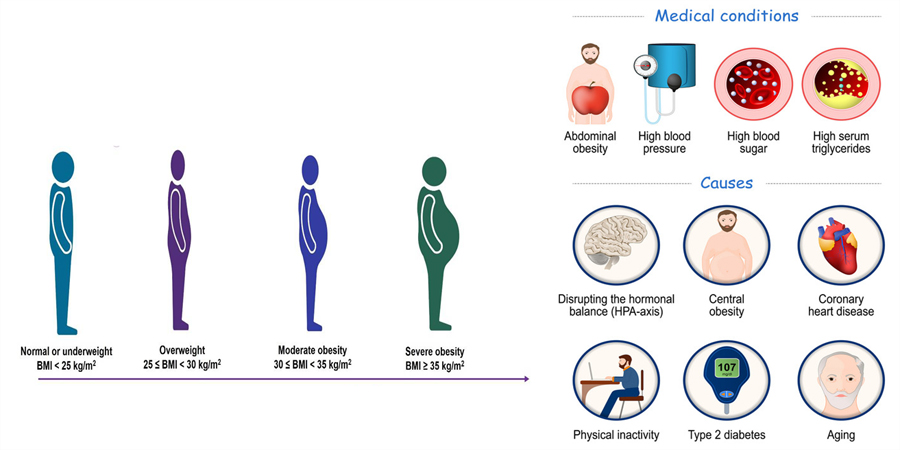
Metabolic syndrome is an important indicator in efforts to control non-communicable diseases. The incidence of metabolic syndrome is directly proportional to the incidence of obesity while the prevalence of metabolic syndrome varies based on sociodemographic characteristics and lifestyle. Efforts to identify metabolic syndrome in the community are a crucial step to identify early the potential for hypertension, coronary heart disease, stroke and diabetes mellitus. This study aims to identify components of metabolic syndrome based on gender. Cross sectional study is the research design that underlies data collection on risk factors for metabolic syndrome which is carried out through interviews and measurements of height, weight, waist circumference, blood pressure and cholesterol levels using NCEP-III criteria as the basis for identifying metabolic syndrome. Data analysis used the Chi-Square test. The metabolic syndrome component in the form of obesity is identified in men and women using different indicators. Both men and women have experienced increases in systolic blood pressure and cholesterol levels. A history of smoking was the only risk factor for metabolic syndrome with a statistically significant difference in proportion between men and women. Behavioral modifications such as eating patterns, rest, and others according to the guidance of the Koran and hadith are needed to minimize the incidence of metabolic syndrome.
Downloads
References
Aini, P. N. I., Hassan, A. H., & Rahim, T. H. (2022). Scoping Review: Analisis Pengaruh Rokok terhadap Faktor Risiko Terjadinya Karsinoma Nasofaring. Bandung Conference Series: Medical Science, 2(1), 847–856. https://doi.org/10.29313/BCSMS.V2I1.1788
Amschler, D. H., & McKenzie, J. F. (2010). Perceived sleepiness, sleep habits and sleep concerns of public school teachers, administrators and other personnel. American Journal of Health Education, 41(2), 102-109. https://doi.org/10.1080/19325037.2010.10599134
Bermudez, V., Olivar, L. C., Torres, W., Navarro, C., Gonzalez, R., Espinoza, C., Morocho, A., Mindiola, A., Chacin, M., Arias, V., Añez, R., Salazar, J., Riaño-Garzon, M., Diaz-Camargo, E., Bautista, M. J., & Rojas, J. (2018). Cigarette smoking and metabolic syndrome components: a cross-sectional study from Maracaibo City, Venezuela. F1000Research, 7. https://doi.org/10.12688/F1000RESEARCH.14571.3
Chew, N. W. S., Ng, C. H., Tan, D. J. H., Kong, G., Lin, C., Chin, Y. H., Lim, W. H., Huang, D. Q., Quek, J., Fu, C. E., Xiao, J., Syn, N., Foo, R., Khoo, C. M., Wang, J. W., Dimitriadis, G. K., Young, D. Y., Siddiqui, M. S., Lam, C. S. P., Muthiah, M. D. (2023). The global burden of metabolic disease: Data from 2000 to 2019. Cell Metabolism, 35(3), 414-428.e3. https://doi.org/10.1016/j.cmet.2023.02.003
Cohen, D., Meloni, A., Cadeddu, C., Cugusi, L., Donataccio, M. P., Deidda, M., Sciomer, S., Gallina, S., Vassalle, C., Moscucci, F., Mercuro, G., & Maffei, S. (2023). Gender Differences and Cardiometabolic Risk: The Importance of the Risk Factors. International Journal of Molecular Sciences, 24(1588), 1–17. https://doi.org/10.3390/ijms24021588
Csongová, M., Volkovová, K., Gajdoš, M., Gurecká, R., Koborová, I., Líšková, A., & Šebeková, K. (2018). Gender-Associated Differences In The Prevalence Of Central Obesity Using Waist Circumference And Waist-To-Height Ratio, And That Of General Obesity, In Slovak Adults. Cent Eur J Public Health, 26(3), 228–233. https://doi.org/10.21101/cejph.a4719
De Lorenzo, A., Del Gobbo, V., Premrov, M. G., Bigioni, M., Galvano, F., & Di Renzo, L. (2007). Normal-weight obese syndrome: early inflammation? The American Journal of Clinical Nutrition, 85(1), 40–45. https://doi.org/10.1093/AJCN/85.1.40
de Souza, J. M., Tebar, W. R., Delfino, L. D., Tebar, F. S., Gobbo, L. A., Franco, M., ... & Christofaro, D. G. (2023). Association of Musculoskeletal Pain With Sedentary Behavior in Public School Teachers: The Role of Habitual Physical Activity. Pain Management Nursing, 24(2), 196-200. https://doi.org/10.1016/j.pmn.2022.08.005
Harlinda, N. M., Khusni, B., Dafa Annafis, R., Basyarahil, R. M., & Fatmaningrum, W. (2022). Relationship between age and gender with cholesterol levels of Taro villagers. World Journal of Advanced Research and Reviews, 2022(01), 255–260. https://doi.org/10.30574/wjarr.2022.13.1.0010
Herningtyas, E. H., & Ng, T. S. (2019). Prevalence and distribution of metabolic syndrome and its components among provinces and ethnic groups in Indonesia. BMC Public Health, 19(1), 1–12. https://doi.org/10.1186/S12889-019-6711-7/FIGURES/3
Izumida, T., Nakamura, Y., Sato, Y., & Ishikawa, S. (2021). Association among age, gender, menopausal status and small dense low-density lipoprotein cholesterol: a cross-sectional study. BMJ Open, 11, 41613. https://doi.org/10.1136/bmjopen-2020-041613
Kamso, S., Purwantyastuti, P., Lubis, D. U., Juwita, R., Robbi, Y. K., & Besral, B. (2011). Prevalensi dan Determinan Sindrom Metabolik pada Kelompok Eksekutif di Jakarta dan Sekitarnya. Kesmas: National Public Health Journal, 6(2), 85–90. https://doi.org/10.21109/KESMAS.V6I2.110
Kim, J. H., Kim, B. J., Hyun, Y. Y., & Kang, J. H. (2020). Association between Secondhand Smoke Exposure and Metabolic Syndrome in 118,609 Korean Never Smokers Verified by Self-Reported Questionnaire and Urine Cotinine. Endocrinology and Metabolism, 35(4), 892–900. https://doi.org/10.3803/ENM.2020.847
Lahav, Y., Kfir, A., & Gepner, Y. (2023). The paradox of obesity with normal weight; a cross-sectional study. Frontiers in Nutrition, 10, 1173488. https://doi.org/10.3389/fnut.2023.1173488
Lasimpala, L., Nuryani, N., Ramadhani, F., & Kau, M. (2021). Gambaran Pola Makan dan Pengetahuan Sindrom Metabolik pada Kelompok Dewasa. Gorontalo Journal of Nutrition and Dietetic, 1(2), 64-73.
Marcus, Y., Segev, E., Shefer, G., Eilam, D., Shenkerman, G., Buch, A., Shenhar-Tsarfaty, S., Zeltser, D., Shapira, I., Berliner, S., & Rogowski, O. (2023). Metabolically Healthy Obesity Is a Misnomer: Components of the Metabolic Syndrome Linearly Increase with BMI as a Function of Age and Gender. Biology, 12(5), 719. https://doi.org/10.3390/BIOLOGY12050719/S1
Naghipour, M., Joukar, F., Nikbakht, H. A., Hassanipour, S., Asgharnezhad, M., Arab-Zozani, M., & Mansour-Ghanaei, F. (2021). High Prevalence of Metabolic Syndrome and Its Related Demographic Factors in North of Iran: Results from the PERSIAN Guilan Cohort Study. International Journal of Endocrinology, 2021. https://doi.org/10.1155/2021/8862456
National Cholesterol Education Program, National Heart, L. and B. I., & National Institutes of Health. (2002). Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation, 106(25), 3143–3421. https://doi.org/10.1161/CIRC.106.25.3143
Ofer, K., Ronit, L., Ophir, A., & Amir, K. (2019). Normal body mass index (BMI) can rule out metabolic syndrome An Israeli cohort study. https://doi.org/10.1097/MD.0000000000014712
Prasetyo, G. L., Fitriani, S. E., Sihotang, D. P., & Zulkania, A. (2018). Potensi Kandungan Aseton Dari Limbah Puntung Rokok. Khazanah: Jurnal Mahasiswa, 10(2). https://journal.uii.ac.id/khazanah/article/view/16650
Rodrigues, M. C. ;, Erika da Silva MacielIII;, Fernando Rodrigues Peixoto QuaresmaIII;, Luis Fernando Castagnino SestiIV;, Laércio da Silva PaivaI;, Hugo Macedo JuniorV;, Francisco Albino de AraújoV;, Fernando Luiz Affonso FonsecaV;, & Fernando AdamiI. (2021). Prevalence and factors associated with metabolic syndrome in a vulnerable population in northern Brazil: a cross-sectional study. Journal of Human Growth and Development, 31(2). http://dx.doi.org/10.36311/jhgd.v31.11410
Rohmani, A., Yazid, N., & Rahmawati, A. A. (2018). Rokok Elektrik dan Rokok Konvensional Merusak Alveolus Paru. Prosiding Seminar Nasional Unimus, 1(0). https://prosiding.unimus.ac.id/index.php/semnas/article/view/21
Romero-Corral, A., Somers, V. K., Sierra-Johnson, J., Korenfeld, Y., Boarin, S., Korinek, J., Jensen, M. D., Parati, G., & Lopez-Jimenez, F. (2010). Normal weight obesity: a risk factor for cardiometabolic dysregulation and cardiovascular mortality. https://doi.org/10.1093/eurheartj/ehp487
Sadarang, R. A. I. (2021). Factors Associated With Quitting Smoking in Indonesia. Journal of Preventive Medicine and Public Health, 54(2), 137–144. https://doi.org/10.3961/JPMPH.20.293
Saklayen, M. G. (2018). The Global Epidemic of the Metabolic Syndrome. Current Hypertension Reports, 20(2). https://doi.org/10.1007/S11906-018-0812-Z
Setiarsih, D., Kardina, R. N., Prilistyo, D. I., Putri, P. H., Nuriannisa, F., & Hisbullah, F. J. (2023, October). Pantau Aktivitas Fisik Dan Lingkar Pinggang Untuk Cegah Sindrom Metabolik Di Kalangan Santriwati PP Al Hidayah 2 Bangkalan. In prosiding seminar nasional pengabdian kepada masyarakat (Vol. 3, No. 1, pp. 231-238).
Solomon, S., & Mulugeta, W. (2019). Disease burden and associated risk factors for metabolic syndrome among adults in Ethiopia. BMC Cardiovascular Disorders, 19(1), 1–8. https://doi.org/10.1186/S12872-019-1201-5/TABLES/6
Sugathan, S., Ali, O., Myint Soe, M., Ismail, S., & Ahmad, W. (2021). Socio demographic and lifestyle factors of metabolic syndrome among adult rural indigenous Malaysian population from Perak State, Malaysia. Saudi Journal of Biological Sciences, 28(8), 4818. https://doi.org/10.1016/J.SJBS.2021.05.011
Suhaema, S., & Masthalina, H. (2015). Pola Konsumsi dengan Terjadinya Sindrom Metabolik. Kesmas: Jurnal Kesehatan Masyarakat Nasional (National Public Health Journal), 9(4), 340–347. https://doi.org/10.21109/KESMAS.V9I4.741
Syifa, F. A. (2023). Faktor Risiko Sindrom Metabolik Pada Pegawai Aparatur Sipil Negara (ASN) di Kota Jambi (Doctoral dissertation, Universitas Jambi).Dietetic, 1(2), 64-73. https://repository.unja.ac.id/50784/
Tharu, B. P., & Tsokos, C. P. (2017). A Statistical Study of Serum Cholesterol Level by Gender and Race. Journal of Research in Health Sciences, 17(3), 386. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7189954/
Copyright (c) 2024 Rimawati Aulia Insani Sadarang, Emmi Bujawati, Dian Rezki Wijaya, Dian Ihwana Ansyar, Bs Titi Haerana, Nildawati Nildawati

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
Authors retain copyright and grant the journal right of first publication with the work simultaneously licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License that allows others to share the work with an acknowledgment of the work's authorship and initial publication in this journal.
Authors are able to enter into separate, additional contractual arrangements for the non-exclusive distribution of the journal's published version of the work (e.g., post it to an institutional repository or publish it in a book), with an acknowledgment of its initial publication in this journal.
Authors are permitted to publish their work online in third parties as it can lead to wider dissemination of the work.




