COVID-19 Infection Wave Mortality from Surveillance Data in The Philippines Using Machine Learning
Abstract
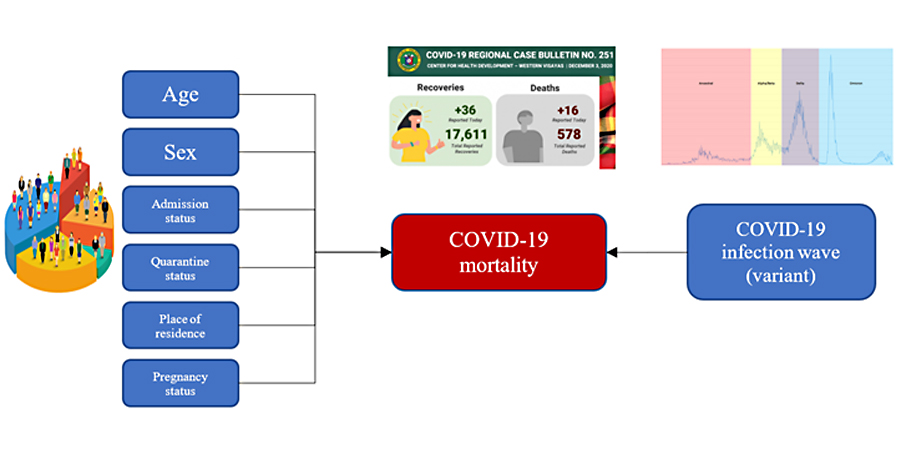
The Philippines had several COVID-19 infection waves brought about by different strains and variants of SARS-CoV-2. This study aimed to describe COVID-19 outcomes by infection waves using machine learning. A cross-sectional surveillance data review design was employed using the DOH COVID Data Drop dataset as of September 24, 2022. The predominant variant(s) of concern divided the dataset into time intervals representing the infection waves: ancestral (A0), Alpha/Beta (AB), Delta (D), and Omicron (O). Descriptive statistics and machine learning models were generated from each infection. The final data set consisted of 3,896,206 cases wherein 98.39% of cases recovered while 1.61% died. The highest and lowest CFR was observed during the ancestral wave (2.49) and the Omicron wave (0.61%), respectively. In all four data sets, higher age groups had higher CFRs, and F-score and specificity were highest using naïve Bayes. Area under the curve (AUC) was highest in the naïve Bayes models for the A0, AB and D models, while sensitivity was highest in the decision tree models for the A0, AB and O models. The ancestral, Alpha/Beta and Delta variants seem to have similar transmission and mortality profiles, while the Omicron variant caused lesser deaths despite increased transmissibility.
Downloads
References
Argosino, F. (2021, November 9). COVID-19 response: A timeline of community quarantine, lockdowns, alert levels. Manila Bulletin. https://mb.com.ph/2021/11/09/covid-19-response-a-timeline-of-community-quarantine-lockdowns-alert-levels/
Bhattacharyya, R. P., & Hanage, W. P. (2022). Challenges in Inferring Intrinsic Severity of the SARS-CoV-2 Omicron Variant. New England Journal of Medicine, 386(7), e14. https://doi.org/10.1056/NEJMp2119682
Bhopal, S. S., & Bhopal, R. (2020). Sex differential in COVID-19 mortality varies markedly by age. The Lancet, 396(10250), 532–533. https://doi.org/10.1016/S0140-6736(20)31748-7
Carbonell, R., Urgelés, S., Rodríguez, A., Bodí, M., Martín-Loeches, I., Solé-Violán, J., Díaz, E., Gómez, J., Trefler, S., Vallverdú, M., Murcia, J., Albaya, A., Loza, A., Socias, L., Ballesteros, J. C., Papiol, E., Viña, L., Sancho, S., Nieto, M., COVID-19 SEMICYUC Working Group. (2021). Mortality comparison between the first and second/third waves among 3,795 critical COVID-19 patients with pneumonia admitted to the ICU: A multicentre retrospective cohort study. The Lancet Regional Health. Europe, 11, 100243. https://doi.org/10.1016/j.lanepe.2021.100243
CDC. (2022, December 28). Risk for COVID-19 Infection, Hospitalization, and Death By Age Group. Centers for Disease Control and Prevention. https://www.cdc.gov/coronavirus/2019-ncov/covid-data/investigations-discovery/hospitalization-death-by-age.html
Christensen, P. A., Olsen, R. J., Long, S. W., Snehal, R., Davis, J. J., Saavedra, M. O., Reppond, K., Shyer, M. N., Cambric, J., Gadd, R., Thakur, R. M., Batajoo, A., Mangham, R., Pena, S., Trinh, T., Kinskey, J. C., Williams, G., Olson, R., Gollihar, J., & Musser, J. M. (2022). Signals of Significantly Increased Vaccine Breakthrough, Decreased Hospitalization Rates, and Less Severe Disease in Patients with Coronavirus Disease 2019 Caused by the Omicron Variant of Severe Acute Respiratory Syndrome Coronavirus 2 in Houston, Texas. The American Journal of Pathology, 192(4), 642–652. https://doi.org/10.1016/j.ajpath.2022.01.007
DOH. (2020). Guidelines on the Risk-Based Public Health Standards for COVID-19 Mitigation (Administrative Order No. 2020-0015). Department of Health. https://www.doh.gov.ph/sites/default/files/health-update/ao2020-0015.pdf
DOH. (2022, October 7). COVID-19 Tracker | Department of Health website. https://doh.gov.ph/covid19tracker
DOH. (2023, February 5). Updates on COVID-19 Vaccines | COVID-19 Vaccination Dashboard. https://doh.gov.ph/vaccines
Endeshaw, Y., & Campbell, K. (2022). Advanced age, comorbidity and the risk of mortality in COVID-19 infection. Journal of the National Medical Association, 114(5), 512–517. https://doi.org/10.1016/j.jnma.2022.06.005
Esper, F. P., Adhikari, T. M., Tu, Z. J., Cheng, Y.-W., El-Haddad, K., Farkas, D. H., Bosler, D., Rhoads, D., Procop, G. W., Ko, J. S., Jehi, L., Li, J., & Rubin, B. P. (2023). Alpha to Omicron: Disease Severity and Clinical Outcomes of Major SARS-CoV-2 Variants. The Journal of Infectious Diseases, 227(3), 344–352. https://doi.org/10.1093/infdis/jiac411
Hu, Z., Huang, X., Zhang, J., Fu, S., Ding, D., & Tao, Z. (2022). Differences in Clinical Characteristics Between Delta Variant and Wild-Type SARS-CoV-2 Infected Patients. Frontiers in Medicine, 8. https://www.frontiersin.org/articles/10.3389/fmed.2021.792135
Hui, K. P. Y., Ho, J. C. W., Cheung, M., Ng, K., Ching, R. H. H., Lai, K., Kam, T. T., Gu, H., Sit, K.-Y., Hsin, M. K. Y., Au, T. W. K., Poon, L. L. M., Peiris, M., Nicholls, J. M., & Chan, M. C. W. (2022). SARS-CoV-2 Omicron variant replication in human bronchus and lung ex vivo. Nature, 603(7902), Article 7902. https://doi.org/10.1038/s41586-022-04479-6
Jiang, Y., Laranjo, J. R., & Thomas, M. (2022). COVID-19 lockdown policy and heterogeneous responses of urban mobility: Evidence from the Philippines. PLOS ONE, 17(6), e0270555. https://doi.org/10.1371/journal.pone.0270555
Johnson, A. G., Amin, A., Ali, A., & et al. (2022). COVID-19 Incidence and Death Rates Among Unvaccinated and Fully Vaccinated Adults with and Without Booster Doses During Periods of Delta and Omicron Variant Emergence—25 U.S. Jurisdictions, April 4–December 25, 2021. MMWR. Morbidity and Mortality Weekly Report, 71. https://doi.org/10.15585/mmwr.mm7104e2
Khera, N., Santesmasses, D., Kerepesi, C., & Gladyshev, V. N. (2021). COVID-19 mortality rate in children is U-shaped. Aging (Albany NY), 13(16), 19954–19962. https://doi.org/10.18632/aging.203442
Kläser, K., Molteni, E., Graham, M., Canas, L. S., Österdahl, M. F., Antonelli, M., Chen, L., Deng, J., Murray, B., Kerfoot, E., Wolf, J., May, A., Fox, B., Capdevila, J., Modat, M., Hammers, A., Spector, T. D., Steves, C. J., Sudre, C. H., Duncan, E. L. (2022). COVID-19 due to the B.1.617.2 (Delta) variant compared to B.1.1.7 (Alpha) variant of SARS-CoV-2: A prospective observational cohort study. Scientific Reports, 12(1), Article 1. https://doi.org/10.1038/s41598-022-14016-0
Lewnard, J. A., Hong, V. X., Patel, M. M., Kahn, R., Lipsitch, M., & Tartof, S. Y. (2022). Clinical outcomes associated with SARS-CoV-2 Omicron (B.1.1.529) variant and BA.1/BA.1.1 or BA.2 subvariant infection in Southern California. Nature Medicine, 28(9), Article 9. https://doi.org/10.1038/s41591-022-01887-z
Lorente-González, M., Suarez-Ortiz, M., & Landete, P. (2022). Evolution and Clinical Trend of SARS-CoV-2 Variants. Open Respiratory Archives, 4(2), 100169. https://doi.org/10.1016/j.opresp.2022.100169
Mahdavi, M., Choubdar, H., Zabeh, E., Rieder, M., Safavi-Naeini, S., Jobbagy, Z., Ghorbani, A., Abedini, A., Kiani, A., Khanlarzadeh, V., Lashgari, R., & Kamrani, E. (2021). A machine learning based exploration of COVID-19 mortality risk. PLOS ONE, 16(7), e0252384. https://doi.org/10.1371/journal.pone.0252384
Malundo, A. F. G., Abad, C. L. R., Salamat, M. S. S., Sandejas, J. C. M., Poblete, J. B., Planta, J. E. G., Morales, S. J. L., Gabunada, R. R. W., Evasan, A. L. M., Cañal, J. P. A., Santos, J. A., Manto, J. T., Mercado, M. E. P., Rojo, R. D., Ornos, E. D. B., & Alejandria, M. M. (2022). Predictors of mortality among inpatients with COVID-19 infection in a tertiary referral center in the Philippines. IJID Regions, 4, 134–142. https://doi.org/10.1016/j.ijregi.2022.07.009
Migriño, J. R., & Batangan, A. R. U. (2021). Using machine learning to create a decision tree model to predict outcomes of COVID-19 cases in the Philippines. Western Pacific Surveillance and Response, 12(3), Article 3. https://doi.org/10.5365/wpsar.2021.12.3.831
Mohsin, M., & Mahmud, S. (2022). Omicron SARS-CoV-2 variant of concern: A review on its transmissibility, immune evasion, reinfection, and severity. Medicine, 101(19), e29165. https://doi.org/10.1097/MD.0000000000029165
Noy, O., Coster, D., Metzger, M., Atar, I., Shenhar-Tsarfaty, S., Berliner, S., Rahav, G., Rogowski, O., & Shamir, R. (2022). A machine learning model for predicting deterioration of COVID-19 inpatients. Scientific Reports, 12(1), Article 1. https://doi.org/10.1038/s41598-022-05822-7
Painuli, D., Mishra, D., Bhardwaj, S., & Aggarwal, M. (2021). Forecast and prediction of COVID-19 using machine learning. Data Science for COVID-19, 381–397. https://doi.org/10.1016/B978-0-12-824536-1.00027-7
Pan, J., St. Pierre, J. M., Pickering, T. A., Demirjian, N. L., Fields, B. K. K., Desai, B., & Gholamrezanezhad, A. (2020). Coronavirus Disease 2019 (COVID-19): A Modeling Study of Factors Driving Variation in Case Fatality Rate by Country. International Journal of Environmental Research and Public Health, 17(21), 8189. https://doi.org/10.3390/ijerph17218189
Rashedi, R., Samieefar, N., Akhlaghdoust, M., Mashhadi, M., Darzi, P., & Rezaei, N. (2022). Delta Variant: The New Challenge of COVID-19 Pandemic, an Overview of Epidemiological, Clinical, and Immune Characteristics. Acta Bio Medica : Atenei Parmensis, 93(1), e2022179. https://doi.org/10.23750/abm.v93i1.12210
Re3data.Org: GISAID. (2022a, October 8). Global COVID-19 submission tracker. GISAID; re3data.org - Registry of Research Data Repositories. https://gisaid.org/submission-tracker-global/
Re3data.Org: GISAID. (2022b, October 8). hCoV-19 Variants Dashboard. GISAID; re3data.org - Registry of Research Data Repositories. https://gisaid.org/hcov-19-variants-dashboard/
Sánchez-Montañés M, Rodríguez-Belenguer P, Serrano-López AJ, Soria-Olivas E, Alakhdar-Mohmara Y. Machine learning for mortality analysis in patients with COVID-19. Int J Environ Res Public Health. 2020. November 12;17(22):8386. 10.3390/ijerph17228386
Serrano, L. G. (2021). Grokking machine learning. Manning Publications.
SeyedAlinaghi, S., Mirzapour, P., Dadras, O., Pashaei, Z., Karimi, A., MohsseniPour, M., Soleymanzadeh, M., Barzegary, A., Afsahi, A. M., Vahedi, F., Shamsabadi, A., Behnezhad, F., Saeidi, S., Mehraeen, E., & Shayesteh Jahanfar. (2021). Characterization of SARS-CoV-2 different variants and related morbidity and mortality: A systematic review. European Journal of Medical Research, 26(1), 51. https://doi.org/10.1186/s40001-021-00524-8
Stein, C., Nassereldine, H., Sorensen, R. J. D., Amlag, J. O., Bisignano, C., Byrne, S., Castro, E., Coberly, K., Collins, J. K., Dalos, J., Daoud, F., Deen, A., Gakidou, E., Giles, J. R., Hulland, E. N., Huntley, B. M., Kinzel, K. E., Lozano, R., Mokdad, A. H., Lim, S. S. (2023). Past SARS-CoV-2 infection protection against re-infection: A systematic review and meta-analysis. The Lancet, 0(0). https://doi.org/10.1016/S0140-6736(22)02465-5
Talabis, D. A. S., Babierra, A. L., Buhat, C. A. H., Lutero, D. S., Quindala, K. M., & Rabajante, J. F. (2021). Local government responses for COVID-19 management in the Philippines. BMC Public Health, 21(1), Article 1. https://doi.org/10.1186/s12889-021-11746-0
Venkatasubramaniam, A., Wolfson, J., Mitchell, N., Barnes, T., JaKa, M., & French, S. (2017). Decision trees in epidemiological research. Emerging Themes in Epidemiology, 14(1), 11. https://doi.org/10.1186/s12982-017-0064-4
Wang, C., Liu, B., Zhang, S., Huang, N., Zhao, T., Lu, Q., & Cui, F. (2022). Differences in incidence and fatality of COVID‐19 by SARS‐CoV‐2 Omicron variant versus Delta variant in relation to vaccine coverage: A world‐wide review. Journal of Medical Virology, 10.1002/jmv.28118. https://doi.org/10.1002/jmv.28118
WHO. (2022, October 4). Tracking SARS-CoV-2 variants. World Health Organization. https://www.who.int/activities/tracking-SARS-CoV-2-variants
WHO. (2023). WHO Coronavirus Disease (COVID-19) Dashboard [Dashboard]. WHO Coronavirus Disease (COVID-19) Dashboard. https://covid19.who.int
Wolter, N., Jassat, W., Walaza, S., Welch, R., Moultrie, H., Groome, M., Amoako, D. G., Everatt, J., Bhiman, J. N., Scheepers, C., Tebeila, N., Chiwandire, N., Plessis, M. du, Govender, N., Ismail, A., Glass, A., Mlisana, K., Stevens, W., Treurnicht, F. K., Cohen, C. (2022). Early assessment of the clinical severity of the SARS-CoV-2 omicron variant in South Africa: A data linkage study. The Lancet, 399(10323), 437–446. https://doi.org/10.1016/S0140-6736(22)00017-4
Yadaw, A. S., Li, Y., Bose, S., Iyengar, R., Bunyavanich, S., & Pandey, G. (2020). Clinical features of COVID-19 mortality: Development and validation of a clinical prediction model. The Lancet Digital Health, 2(10), e516–e525. https://doi.org/10.1016/S2589-7500(20)30217-X
Copyright (c) 2024 Julius Migrino, Ani Regina U. Batangan, Rizal Michael R. Abello

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
Authors retain copyright and grant the journal right of first publication with the work simultaneously licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License that allows others to share the work with an acknowledgment of the work's authorship and initial publication in this journal.
Authors are able to enter into separate, additional contractual arrangements for the non-exclusive distribution of the journal's published version of the work (e.g., post it to an institutional repository or publish it in a book), with an acknowledgment of its initial publication in this journal.
Authors are permitted to publish their work online in third parties as it can lead to wider dissemination of the work.