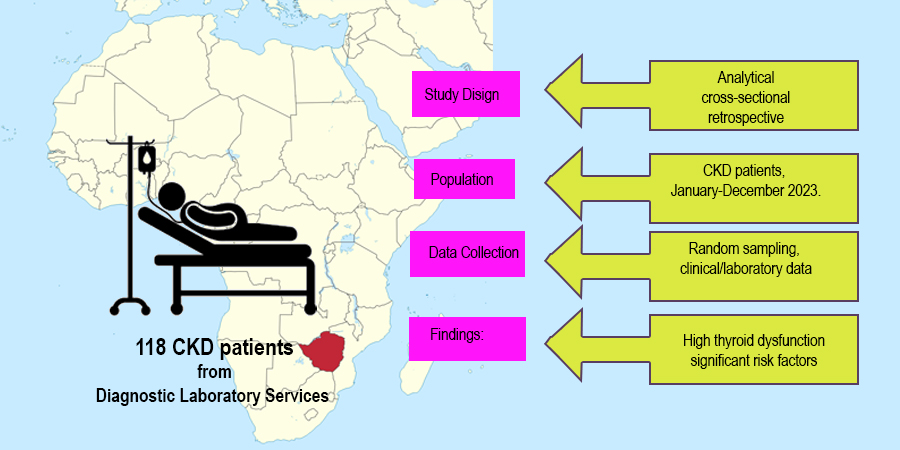
Prevalence of Thyroid Dysfunction among Patients with Chronic Kidney Disease Attending Diagnostic Laboratory Services, Bulawayo, Zimbabwe
Abstract
Chronic kidney disease (CKD), can alter thyroid hormone production, distribution, and excretion. Thyroid dysfunctions like hypothyroidism, hyperthyroidism, and euthyroidism are identified in renal failure patients. This study aimed to determine thyroid dysfunction prevalence among CKD patients who attended Diagnostic Laboratory Services in Bulawayo from January to December 2023. The study was analytical cross-sectional and archival data collection methods were to gather information from 118 CKD patients who underwent both thyroid function tests and urea and electrolytes tests. A descriptive and analytical statistic test was used to determine the prevalence of thyroid dysfunction among CKD patients Chi square test was used to test association between thyroid’s dysfunction in CKD setting with various risk factors, P< 0.05 was considered as statistically significant. Thyroid dysfunction (TD) prevalence was 53%, increasing with CKD severity, with stage 3B having a high prevalence of 37%. Major types include subclinical hypothyroidism (11%), overt hypothyroidism (16%), and subclinical hyperthyroidism (4.2%), with 36% of females presenting with thyroid dysfunction as compared to 31% of males. Prevalence of thyroid dysfunction increased with an increase in age Majors risk factor for CKD in TD setting were hypertension, diabetes, and heart failure. In conclusion, there was a high prevalence of thyroid dysfunction (53%) among chronic kidney disease patients.
Downloads
References
Ansari, I., Kumar, S., Acharya, S., Agrawal, S., & Saboo, K. (2023). Thyroid dysfunction at different stages of chronic kidney disease: a cross-sectional study at a rural teaching college in central India. Cureus, 15(7). https://doi.org/10.7759%2Fcureus.42130
Bikbov, B., Purcell, C. A., Levey, A. S., Smith, M., Abdoli, A., Abebe, M., & Owolabi, M. O. (2020). Global, regional, and national burden of chronic kidney disease, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. The lancet, 395(10225), 709-733. https://doi.org/10.1016/S0140-6736(20)30045-3
Cotoi, L., Borcan, F., Sporea, I., Amzar, D., Schiller, O., Schiller, A., Stoian, D. (2020). Thyroid Pathology in End-Stage Renal Disease Patients on Hemodialysis. Diagnostics (Basel), 10(4). http//doi.org/10.3390/diagnostics10040245
Chonchol, M., Cigolini, M., & Targher, G. (2008). Association between 25-hydroxyvitamin D deficiency and cardiovascular disease in type 2 diabetic patients with mild kidney dysfunction. Nephrology Dialysis Transplantation, 23(1), 269-274. https://doi.org/10.1093/ndt/gfm537
Heidari, Z., & Asadzadeh, R. (2021). Subclinical hypothyroidism is a risk factor for diabetic retinopathy in patients with type 2 diabetes mellitus. Medical Journal of the Islamic Republic of Iran, 35. https://doi.org/10.47176%2Fmjiri.35.186
Hunter-Dickson, M., Drak, D., Anderson, M., Shamu, T., Chimbetete, C., Dahwa, R., & Gracey, D. M. (2023). Comparison of CG, CKD-EPI[AS] and CKD-EPI[ASR] equations to estimate glomerular filtration rate and predict mortality in treatment naïve people living with HIV in Zimbabwe. BMC Nephrology, 24(1), 129. http//doi.org/10.1186/s12882-023-03159-5
Kashif, M., Hussain, M. S., Anis, M., & Shah, P. K. (2023). Thyroid Dysfunction and Chronic Kidney Disease: A Study Among the Northeastern Population of India. Cureus, 15(5). https://doi.org/10.7759%2Fcureus.38700
Keunmoe, P., Halle, M. P., & Nguedia, J. C. A. (2019). Correlation Between Biomarkers of Thyroid Function Abnormalities and Stages of Chronic Kidney Disease in Cameroon. J Med-Clin Res & Rev, 3(6), 1-8.
Kher, V. (2002). End-stage renal disease in developing countries. Kidney international, 62(1), 350-362. https://doi.org/10.1046/j.1523-1755.2002.00426.x
Klein, I., & Ojamaa, K. (2001). Thyroid hormone and the cardiovascular system. New England Journal of Medicine, 344(7), 501-509. http//doi.org/10.1056/NEJM2001021534407
Levin, A., & Stevens, P. E. (2014). Summary of KDIGO 2012 CKD Guideline: behind the scenes, need for guidance, and a framework for moving forward. Kidney international, 85(1), 49-61. https://doi.org/10.1038/ki.2013.444
Li, L.Z., Hu, Y., Ai, S.-L., Cheng, L., Liu, J., Morris, E., Fu, P. (2019). The relationship between thyroid dysfunction and nephrotic syndrome: a clinicopathological study. Scientific reports, 9(1), 6421. https://doi.org/10.1038/s41598-019-42905-4
Liu, L., Zeng, B., Zhang, J., Li, G., & Zong, W. (2023). Impact of subclinical hypothyroidism on in-hospital outcomes and long-term mortality among acute myocardial infarction patients with diabetic mellitus. Acta Cardiologica, 1-9. https://doi.org/10.1080/00015385.2023.2279421
Lo, J. C., Chertow, G. M., Go, A. S., & Hsu, C.-Y. (2005). Increased prevalence of subclinical and clinical hypothyroidism in persons with chronic kidney disease. Kidney international, 67(3), 1047-1052. https://doi.org/10.1111/j.1523-1755.2005.00169.x
Lv, J.C., & Zhang, L.X. (2019). Prevalence and disease burden of chronic kidney disease. Renal fibrosis: mechanisms and therapies, 3-15. https://doi.org/10.1007/978-981-13-8871-2_1
McGrogan, A., Seaman, H. E., Wright, J. W., & De Vries, C. S. (2008). The incidence of autoimmune thyroid disease: a systematic review of the literature. Clinical endocrinology, 69(5), 687-696. https://doi.org/10.1111/j.1365-2265.2008.03338.x
Mohamedali, M., Reddy Maddika, S., Vyas, A., Iyer, V., & Cheriyath, P. (2014). Thyroid disorders and chronic kidney disease. Int J Nephrol, 2014, 520281. http//doi.org/10.1155/2014/520281
Mudie, K., Jin, M. M., Kendall, L., Addo, J., dos-Santos-Silva, I., Quint, J., & Natamba, B. (2019). Non-communicable diseases in sub-Saharan Africa: a scoping review of large cohort studies. Journal of global health, 9(2). https://doi.org/10.7189%2Fjogh.09.020409
Narasaki, Y., Sohn, P., & Rhee, C. M. (2021). The Interplay Between Thyroid Dysfunction and Kidney Disease. Semin Nephrol, 41(2), 133-143. http//doi.org/10.1016/j.semnephrol.2021.03.008
Raj, R., Kumar, V., Bhushan, D., Biswas, R., & Ojha, V. S. (2023). The prevalence of thyroid abnormalities in patients with chronic kidney disease: A cross-sectional study at a tertiary care hospital. Cureus, 15(8). https://doi.org/10.7759%2Fcureus.43065
Rashad, N. M., & Samir, G. M. (2019). Prevalence, risks, and comorbidity of thyroid dysfunction: a cross-sectional epidemiological study. The Egyptian Journal of Internal Medicine, 31(4), 635-641. http//doi.org/10.4103/ejim.ejim_22_19
Rhee, C. M. (2015). Low-T3 syndrome in peritoneal dialysis: metabolic adaptation, marker of illness, or mortality mediator? Clinical Journal of the American Society of Nephrology, 10(6), 917-919. https://doi.org/10.2215/CJN.04310415
Rhee, C. M. (2019). Thyroid disease in end-stage renal disease. Curr Opin Nephrol Hypertens, 28(6), 621-630. http//doi.org/10.1097/mnh.0000000000000542
Rhee, C. M., Brent, G. A., Kovesdy, C. P., Soldin, O. P., Nguyen, D., Budoff, M. J., & Kalantar-Zadeh, K. (2015). Thyroid functional disease: an under-recognized cardiovascular risk factor in kidney disease patients. Nephrology Dialysis Transplantation, 30(5), 724-737. https://doi.org/10.1093/ndt/gfu024
Rhee, C. M., Kalantar-Zadeh, K., Streja, E., Carrero, J.-J., Ma, J. Z., Lu, J. L., & Kovesdy, C. P. (2015). The relationship between thyroid function and estimated glomerular filtration rate in patients with chronic kidney disease. Nephrology Dialysis Transplantation, 30(2), 282-287. https://doi.org/10.1093/ndt/gfu303
Schultheiss, U. T., Steinbrenner, I., Nauck, M., Schneider, M. P., Kotsis, F., Baid-Agrawal, S., & GCKD investigators. (2021). Thyroid function, renal events and mortality in chronic kidney disease patients: the German Chronic Kidney Disease study. Clinical Kidney Journal, 14(3), 959-968. https://doi.org/10.1093/ckj/sfaa052
Shakya, S., Kumar, S., Verma, V., Gupta, H., Sonkar, S. K., & Atam, V. (2023). Evaluation of Interactions Between Thyroid Dysfunction in End-Stage Renal Disease Patients: A Cross-Sectional Study. Cureus, 15(2). https://doi.org/10.7759%2Fcureus.35088
Srivastava, S., Rajput, J., Shrivastava, M., Chandra, R., Gupta, M., & Sharma, R. (2018). Correlation of thyroid hormone profile with biochemical markers of renal function in patients with undialyzed chronic kidney disease. Indian Journal of Endocrinology and Metabolism, 22(3), 316-320. https://doi.org/10.4103/ijem.ijem_475_17
Stöhr, W., Walker, A. S., Munderi, P., Tugume, S., Gilks, C. F., Darbyshire, J. H., & Hakim, J. (2008). Estimating glomerular filtration rate in HIV-infected adults in Africa: Comparison of Cockcroft–Gault and Modification of Diet in Renal Disease formulae. Antiviral therapy, 13(6), 761-770. https://doi.org/10.1177/135965350801300613
Stoian, D., Borcan, F., Petre, I., Mozos, I., Varcus, F., Ivan, V., Dehelean, C. A. (2019). Strain elastography as a valuable diagnosis tool in intermediate cytology (Bethesda III) thyroid nodules. Diagnostics, 9(3), 119. https://doi.org/10.3390/diagnostics9030119
Stoian, D., Ivan, V., Sporea, I., Florian, V., Mozos, I., Navolan, D., & Nemescu, D. (2020). Advanced ultrasound application–Impact on presurgical risk stratification of the thyroid nodules. Therapeutics and Clinical Risk Management, 21-30. https://doi.org/10.2147/TCRM.S224060
Taylor, P. N., Albrecht, D., Scholz, A., Gutierrez-Buey, G., Lazarus, J. H., Dayan, C. M., & Okosieme, O. E. (2018). Global epidemiology of hyperthyroidism and hypothyroidism. Nature Reviews Endocrinology, 14(5), 301-316. https://doi.org/10.1038/nrendo.2018.18
Thomas, R., Kanso, A., & Sedor, J. R. (2008). Chronic kidney disease and its complications. Prim Care, 35(2), 329-344, vii. http//doi.org/10.1016/j.pop.2008.01.008
Yang, C., Wang, H., Zhao, X., Matsushita, K., Coresh, J., Zhang, L., & Zhao, M. H. (2020). CKD in China: evolving spectrum and public health implications. American Journal of Kidney Diseases, 76(2), 258-264. https://doi.org/10.1053/j.ajkd.2019.05.032
Copyright (c) 2024 Lindwe Angela Sibanda, Sundika Makengo Olivier, Idi Doutchi Yacoubou, Aboubacar Katiella Kaka, Maibouge Tanko Mahamane Salissou

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
Authors retain copyright and grant the journal right of first publication with the work simultaneously licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License that allows others to share the work with an acknowledgment of the work's authorship and initial publication in this journal.
Authors are able to enter into separate, additional contractual arrangements for the non-exclusive distribution of the journal's published version of the work (e.g., post it to an institutional repository or publish it in a book), with an acknowledgment of its initial publication in this journal.
Authors are permitted to publish their work online in third parties as it can lead to wider dissemination of the work.