Incidence of Cervicitis in Infertile Women: A Study in Medical Center Clinic, Makassar City, Indonesia
Abstract
Infertility is a significant global health concern, yet the role of cervicitis as an independent risk factor remains inadequately explored. While previous studies have investigated various causes of infertility, limited research has specifically examined the combined effect of cervicitis and sperm abnormalities on reproductive outcomes. This study aims to determine the impact of cervicitis on infertility and assess its association with sperm abnormalities among married couples seeking conception. A cross-sectional study was conducted at the Wirahusada Medical Center Clinic, Makassar, Indonesia, involving 94 married couples undergoing routine fertility assessments. Cervicitis was diagnosed through endoscopic examination, while sperm abnormalities—including oligospermia, poor motility, and abnormal morphology—were identified via semen analysis following WHO 2021 standards. The odds ratio (OR) and Chi-Square test were used to analyze the relationship between cervicitis, sperm abnormalities, and infertility. Women with cervicitis had a lower pregnancy rate (25% vs. 75%), with an infertility risk 7.186 times higher (OR = 7.186). Men with sperm abnormalities also had a higher infertility risk (OR = 4.234). The highest risk (OR = 9.060) was in couples where both partners had these conditions. This study highlights the significant impact of cervicitis on female infertility, particularly when accompanied by sperm abnormalities. These findings underscore the need for integrated reproductive health strategies, including early screening and targeted interventions, to enhance pregnancy success rates among couples facing infertility.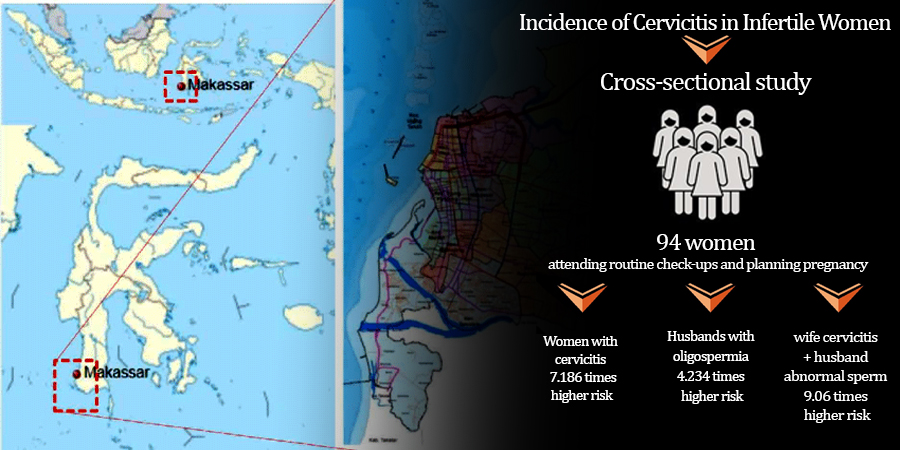
Downloads
References
Adefuye, A. O., Adeola, H. A., Sales, K. J., & Katz, A. A. (2016). Seminal fluid‐mediated inflammation in physiology and pathology of the female reproductive tract. Journal of immunology research, 2016(1), 9707252. http://dx.doi.org/10.1155/2016/9707252
Arshad, N., Naeem, M., Bilal, M., Aftab, S., & Mahrukh, F. (2023). Cervical abnormalities are related to infertility: a review. Lahore Garrison University Journal of Life Sciences, 7(01), 108-119. https://doi.org/10.54692/lgujls.2023.0701242
Azzahra, F. (2022). Infertilitas Dan Penanganannya Dalam Al-Qur’an (Doctoral dissertation, Institut PTIQ Jakarta). https://repository.ptiq.ac.id/id/eprint/933/
Bazzazan, A. (2024). Diagnosis of clinical cervicitis and vaginitis in dairy cows in relation to various postpartum uterine disorders. Clinical Theriogenology, 16. https://doi.org/10.58292/ct.v16.10309
Biggs, S., Kennedy, J., Lewis, S., Hearps, S., McLachlan, R., Saldern, S., & Halliday, J. (2023). Lifestyle and environmental risk factors for unexplained male infertility: study protocol for australian male infertility exposure (amie), a case–control study. Reproductive Health, 20(1). https://doi.org/10.1186/s12978-023-01578-z
Bisht, S., Banu, S., Srivastava, S., Pathak, R., Kumar, R., Dada, R., & Mishra, R. (2020). Sperm methylome alterations following yoga‐based lifestyle intervention in patients of primary male infertility: a pilot study. Andrologia, 52(4). https://doi.org/10.1111/and.13551
Cannarella, R., Condorelli, R., Mongioì, L., Vignera, S., & Calogero, A. (2020). Molecular biology of spermatogenesis: novel targets of apparently idiopathic male infertility. International Journal of Molecular Sciences, 21(5), 1728. https://doi.org/10.3390/ijms21051728
Castleton, P., Deluao, J., Sharkey, D., & McPherson, N. (2022). Measuring reactive oxygen species in semen for male preconception care: a scientist perspective. Antioxidants, 11(2), 264. https://doi.org/10.3390/antiox11020264
Chen, R., Fu, Y., You, B., Liu, Y., Yao, Y., Wang, X., & Cheng, X. (2021). Clinical characteristics of single human papillomavirus 53 infection: a retrospective study of 419 cases. BMC Infectious Diseases, 21(1). https://doi.org/10.1186/s12879-021-06853-7
D’Amato, A. (2024). Reproductive outcomes in young women with early-stage cervical cancer greater than 2 cm undergoing fertility-sparing treatment: a systematic review. Medicina, 60(4), 608. https://doi.org/10.3390/medicina60040608
D'Amico, M. (2023). Chlamydia trachomatis–specific antibody responses in women in cameroon with secondary infertility. Sexually Transmitted Diseases, 50(11), e30-e33. https://doi.org/10.1097/olq.0000000000001866
Devi, S. (2024). Clinical characteristics and colposcopy appearance of cervical intraepithelial neoplasia. International Journal of Reproduction Contraception Obstetrics and Gynecology, 13(2), 224-228. https://doi.org/10.18203/2320-1770.ijrcog20240113
Dong, Y., Zhong, F., Zhang, N., Shao, J., Shen, J., Yang, E., & Li, X. (2023). Urogenital tract and rectal microbiota composition and its influence on reproductive outcomes in infertile patients. Frontiers in Microbiology, 14. https://doi.org/10.3389/fmicb.2023.1051437
Fayyaz, A., Tabassum, S., & Qadir, S. (2020). Frequency of male factor and abnormalities of semen analysis in infertile couple.. The Professional Medical Journal, 27(07), 1454-1458. https://doi.org/10.29309/tpmj/2020.27.07.4280
Garg, J., Meena, R., Shukla, S., Sharma, S., & Choudhury, R. (2020). Abnormal semen parameters among males in infertile couples: a cross sectional study from a tertiary care centre. International Journal of Reproduction Contraception Obstetrics and Gynecology, 9(8), 3398. https://doi.org/10.18203/2320-1770.ijrcog20203330
Graspeuntner, S., Bohlmann, M., Gillmann, K., Speer, R., Kuenzel, S., Mark, H., & Rupp, J. (2018). Microbiota-based analysis reveals specific bacterial traits and a novel strategy for the diagnosis of infectious infertility. Plos One, 13(1), e0191047. https://doi.org/10.1371/journal.pone.0191047
Gupta, G. and Gupta, A. (2019). Assessment of cervical cytomorphological changes in infertile women. International Journal of Medical and Biomedical Studies, 3(3). https://doi.org/10.32553/ijmbs.v3i3.145
Hassan, Q., Mufti, A., & Mufti, S. (2022). Seroprevalence of chlamydia trachomatis infection in kashmiri women of reproductive age with mucopurulent cervicitis, infertility and ectopic pregnancy - a hospital based study. International Journal of Reproduction Contraception Obstetrics and Gynecology, 11(2), 563. https://doi.org/10.18203/2320-1770.ijrcog20220188
Hussain, S., Hariprasad, R., Dhanasekaran, K., Verma, S., Agarwal, V., Sandeep, .., & Gupta, S. (2022). High prevalence of cervical high-grade lesions and high-risk human papillomavirus infections in women living with hiv: a case for prioritizing cervical screening in this vulnerable group. Acta Cytologica, 66(6), 496-506. https://doi.org/10.1159/000525340
Iarova, I. (2024). The role of cd138 immunohistochemical marker in the diagnosis of chronic endometritis: causes of female infertility. FEM, 27-37. https://doi.org/10.57125/fem.2024.03.30.03
Karavolos, S., Panagiotopoulou, N., AlAhwany, H., & Silva, S. (2020). An update on the management of male infertility. The Obstetrician & Gynaecologist, 22(4), 267-274. https://doi.org/10.1111/tog.12688
Khalifa, E., Fayk, A., Rashad, E., & Aly, A. (2018). Hysteroscopic detection of intrauterine pathology in women with unexplained infertility. The Medical Journal of Cairo University, 86(6), 1287-1294. https://doi.org/10.21608/mjcu.2018.56294
Khandelwal, M. (2023). Establishing the taxa with phylogenetic profile and in-silico ayurvedic remedy of cervicitis microbiome., 201-220. https://doi.org/10.2991/978-94-6463-164-7_15
Kunev, A. (2019). Diagnostics and treatment of cervical causes of infertility. Journal of Biomedical and Clinical Research, 12(1), 33-39. https://doi.org/10.2478/jbcr-2019-0005
Lee, S., Lee, T., Song, S., Kim, D., Choi, K., Lee, J., & Kim, D. (2021). Update on genetic screening and treatment for infertile men with genetic disorders in the era of assisted reproductive technology. Clinical and Experimental Reproductive Medicine, 48(4), 283-294. https://doi.org/10.5653/cerm.2021.04476
Maegawa, M., Kamada, M., Irahara, M., Yamamoto, S., Yoshikawa, S., Kasai, Y., & Aono, T. (2002). A repertoire of cytokines in human seminal plasma. Journal of Reproductive Immunology, 54(1-2), 33-42. https://doi.org/10.1016/S0165-0378(01)00063-8
Moragianni, D., Dryllis, G., Andromidas, P., Kapeta-Korkouli, R., Kouskouni, E., Pessach, I., & Baka, S. (2019). Genital tract infection and associated factors affect the reproductive outcome in fertile females and females undergoing in vitro fertilization. Biomedical Reports. https://doi.org/10.3892/br.2019.1194
Musa, N. (2024). Preventable male infertility: identifying the modifiable risk factors. Journal of Saidu Medical College Swat, 14(2), 79-83. https://doi.org/10.52206/jsmc.2024.14.2.833
Nevezhkina, T. (2023). Evaluation of the influence of inosine pranobex on the matrix protein system in patients with chronic viral cervicitis. Medical Immunology (Russia), 25(4), 863-870. https://doi.org/10.15789/1563-0625-eot-2697
Pavuluri, H. (2024). Oxidative stress-associated male infertility: current diagnostic and therapeutic approaches. Medicina, 60(6), 1008. https://doi.org/10.3390/medicina60061008
Sharkey, D. J., Tremellen, K. P., Jasper, M. J., Gemzell-Danielsson, K., & Robertson, S. A. (2012). Seminal fluid induces leukocyte recruitment and cytokine and chemokine mRNA expression in the human cervix after coitus. The Journal of Immunology, 188(5), 2445-2454. https://doi.org/10.4049/jimmunol.1102736
Sheikh, I., Beg, M., Hamoda, T., Mandourah, H., & Memili, E. (2023). Androgen receptor signaling and pyrethroids: potential male infertility consequences. Frontiers in Cell and Developmental Biology, 11. https://doi.org/10.3389/fcell.2023.1173575
Sherpa, A., Singh, N., Bajracharya, M., Pradhan, A., & Pradhan, P. (2019). Reproductive health status of married women participating in cervical cancer screening in kathmandu. Journal of Chitwan Medical College, 9(2), 30-35. https://doi.org/10.3126/jcmc.v9i2.24528
Thaker, N. (2023). The role of transvaginal sonography in diagnosis of female infertility: a study protocol. F1000research, 12, 1335. https://doi.org/10.12688/f1000research.140962.1
Vries, C. (2024). The psychosocial impact of male infertility on men undergoing icsi treatment: a qualitative study. Reproductive Health, 21(1). https://doi.org/10.1186/s12978-024-01749-6
Xin, T., Ge, S., Chen, L., Cai, L., Hwang, M., & Wang, C. (2018). Relationships between female infertility and female genital infections and pelvic inflammatory disease: a population-based nested controlled study. Clinics, 73, e364. https://doi.org/10.6061/clinics/2018/e364
Yousuf, S., Ikram, A., Ikram, S., Nadeem, S., Hussain, S., & Ali, S. (2022). Chlamydia trachomatis–a cause of infertility at tertiary care hospital, pakistan. Pakistan Armed Forces Medical Journal, 72(4), 1202-05. https://doi.org/10.51253/pafmj.v72i4.3166
Yu, J., Zhou, Y., Luo, H., Su, X., Tian, G., Wang, J., & He, J. (2023). Mycoplasma genitalium infection in the female reproductive system: diseases and treatment. Frontiers in Microbiology, 14. https://doi.org/10.3389/fmicb.2023.1098276
Zang, L. (2024). Relationship between vaginal microecology and human papillomavirus infection as well as cervical intraepithelial neoplasia in 2,147 women from wenzhou, the southeast of china. Frontiers in Oncology, 13. https://doi.org/10.3389/fonc.2023.1306376
Zuend, C., Lamont, A., Noël‐Romas, L., Knodel, S., Birse, K., Kratzer, K., & Burgener, A. (2023). Increased genital mucosal cytokines in canadian women associate with higher antigen-presenting cells, inflammatory metabolites, epithelial barrier disruption, and the depletion of l. crispatus. Microbiome, 11(1). https://doi.org/10.1186/s40168-023-01594-y
Copyright (c) 2025 Dewi Setiawati, Novianeu Salsabila Rachma

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
Authors retain copyright and grant the journal right of first publication with the work simultaneously licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License that allows others to share the work with an acknowledgment of the work's authorship and initial publication in this journal.
Authors are able to enter into separate, additional contractual arrangements for the non-exclusive distribution of the journal's published version of the work (e.g., post it to an institutional repository or publish it in a book), with an acknowledgment of its initial publication in this journal.
Authors are permitted to publish their work online in third parties as it can lead to wider dissemination of the work.