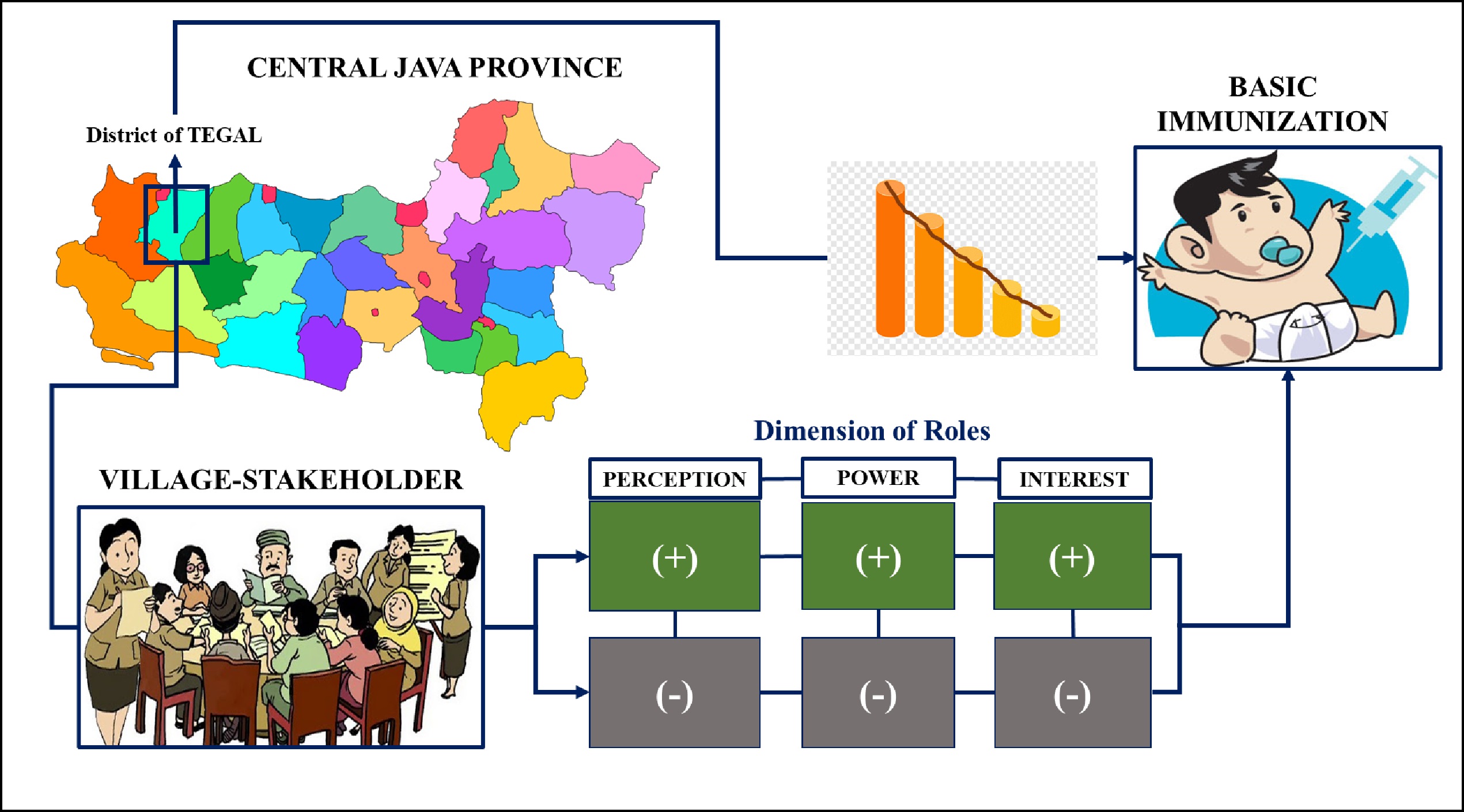
Roles of Village Stakeholders on Immunization Program during Pandemic Outbreak in Central Java, Indonesia
Abstract
Tegal district is facing obstacles in achieving immunization targets during the Covid-19 pandemic as the declining number of children who have been immunized. The role and support of village stakeholders considerably play a very significant role in overcoming these obstacles. This current study aimed to analyze the dimensions of village stakeholders’ roles in achieving basic immunization targets during the pandemic era. This study was conducted using a quantitative survey with a cross-sectional approach. The participants were all village stakeholders related to the immunization program. There were 300 people from 30 selected villages as samples chosen through a purposive technique sampling. The roles of stakeholders were found to be the dimensions of perceptions, powers, and respectively interests. The results were most of the stakeholders showed such positive dimensions of perception related to their roles in immunization as well as interest dimensions. All respondents, in addition, considered that their institutions have no power in implementing immunization programs in villages. The immunization success was the responsibility of PHC and health workers instead. There was a relationship between perceptions with strengths and interests, as well as a relationship between strengths with interests of village stakeholders in the immunization program (p<0.05). The weakest role of village stakeholders was in the power dimension as they rely highly on the local governments and health workers with a weak authority to make decisions. Thus, strengthening the role needs to be done through continuous socialization and dissemination with interactive coordination methods, and direct and personal communication.
Downloads
References
Agócs, M., Ismail, A., Kamande, K., Tabu, C., Momanyi, C., Sale, G., Rhoda, D. A., Khamati, S., Mutonga, K., Mitto, B., & Hennessey, K. (2021). Reasons why children miss vaccinations in Western Kenya; A step in a five-point plan to improve routine immunization. Vaccine, 39(34), 4895–4902. https://doi.org/10.1016/j.vaccine.2021.02.071
Arifada, A. Y., & Rochmah, T. N. (2015). Analisis Sistem Kemitraan dalam Program Imunisasi Berdasarkan Peran Perangkat Desa, Bidan Desa dan Masyarakat. Jurnal Administrasi Kesehatan Indonesia, 3(2), 139–150. https://doi.org/10.1145/3132847.3132886
Ayiko, R., Basheka, B., Kareija, G., Pontious, A., Nelson, D., Anguyo Onzima, R., Sreeramareddy, C., Govule, P., Rogers, A., Benon, B., Gerald, K., Robert Onzima, A., Chandrashekhar, S., & Philip, G. (2015). Perspectives of Local Government Stakeholders on Utilization of Maternal and Child Health Services; and Their Roles in North Western Uganda. International Journal of Public Health Research, 3(4), 135–144. http://www.openscienceonline.com/journal/ijphr
Buccini, G., Harding, K. L., Eguiluz, I. F., Safon, C. B., Hromi-Fielder, A., De Cosio, T. G., & P rez-Escamilla, R. (2020). An analysis of stakeholder networks to support the breastfeeding scale-up environment in Mexico. Journal of Nutritional Science, 9(10), 1–10. https://doi.org/10.1017/jns.2020.4
Ekirapa-Kiracho, E., Ghosh, U., Brahmachari, R., & Paina, L. (2017). Engaging stakeholders: Lessons from the use of participatory tools for improving maternal and child care health services. Health Research Policy and Systems, 15(Suppl 2), 17–28. https://doi.org/10.1186/s12961-017-0271-z
Febriastuti, N., Arif, Y. S., & Kusumaningrum, T. (2014). Kepatuhan Orang Tua dalam Pemberian Kelengkapan Imunisasi Dasar pada Bayi 4-11 Bulan. Pediomaternal Nursing, 031, 1–15. https://ojs2.e-journal.unair.ac.id/PMNJ/article/view/11793
Felicia, F. V., & Suarca, I. K. (2020). Pelayanan Imunisasi Dasar pada Bayi di Bawah Usia 12 Bulan dan Faktor yang Memengaruhi di RSUD Wangaya Kota Denpasar Selama Masa Pandemi COVID-19. Sari Pediatri, 22(133), 139–145.
Fisabililah, F. F. N., Nisaq, A. R., & Nurrahmawati, S. (2020). Pengelolaan Dana Desa dalam Pemberdayaan Masyarakat. JIAP (Jurnal Ilmu Administrasi Publik), 8(1), 208. https://doi.org/10.31764/jiap.v8i1.1932
Fisher, M. P., Gurfinkel, D., Szilagyi, P. G., Saville, A., Albertin, C., Breck, A., Valderrama, R., & Kempe, A. (2019). Supporting and sustaining centralized reminder/recall for immunizations: Qualitative insights from stakeholders. Vaccine, 37(44), 6601–6608. https://doi.org/10.1016/j.vaccine.2019.09.055
Irawati, N. A. V. (2020). Imunisasi Dasar dalam Masa Pandemi COVID-19. Jurnal Kedokteran Universitas Lampung, 4(2), 205–210. https://juke.kedokteran.unila.ac.id/index.php/JK/article/view/2898/
Ismawati, L., Sriatmi, A., & Fatmasari, E. Y. (2017). Analisis Peran Pemerintah Desa dalam Penyusunan Anggaran dana Desa untuk Pengembangan Kesehatan di Posyandu Kecamatan Srengat Kabupaten Blitar. Jurnal Kesehatan Masyarakat, 5(1), 75–84. https://ejournal3.undip.ac.id/index.php/jkm/article/view/14875/14391
Iswarno, I., Hasanbasri, M., & Lazuardi, L. (2013). Analisis Untuk Penerapan Kebijakan: Analisis Stakeholder Dalam Kebijakan Program Kesehatan Ibu Dan Anak Di Kabupaten Kepahiang. Jurnal Kebijakan Kesehatan Indonesia, 2(02), 77–85. https://jurnal.ugm.ac.id/jkki/article/view/3218
Kapiriri, L., & Razavi, D. S. (2021). Salient stakeholders: Using the salience stakeholder model to assess stakeholders’ influence in healthcare priority setting. Health Policy OPEN, 2(May), 1–7. https://doi.org/10.1016/j.hpopen.2021.100048
Kartini, E., Kiswanto, Hanafi, A., Nurmaimun, & Rany, N. (2020). The Analysis of Stakeholders Role ’ s in the Children Under-five Years Nutrition Program in Kampar. Jurnal Kesehatan Komunitas, 6(2), 243–247. https://jurnal.htp.ac.id/index.php/keskom/article/view/541
Kementerian Kesehatan & UNICEF Indonesia. (2020). Imunisasi Rutin Anak Selama Pandemi COVID-19 di Indonesia: Persepsi Orang tua dan Pengasuh (pp. 1–16). https://www.unicef.org/indonesia/media/6071/file/
Lyu, J., Miao, T., Dong, J., Cao, R., Li, Y., & Chen, Q. (2020). Reflection on lower rates of COVID-19 in children : Does childhood immunizations o ff er unexpected protection ? Medical Hypotheses, 143(109842), 1–6. https://doi.org/10.1016/j.mehy.2020.109842
Mugali, R. R., Mansoor, F., Parwiz, S., Ahmad, F., Safi, N., Higgins-Steele, A., & Varkey, S. (2017). Improving immunization in Afghanistan: results from a cross-sectional community-based survey to assess routine immunization coverage. BMC Public Health, 17(1), 1–9. https://doi.org/10.1186/s12889-017-4193-z
Namazzi, G., Kiwanuka, S. N., Peter, W., John, B., Olico, O., Allen, K. A., Hyder, A. A., & Ekirapa, K. E. (2013). Stakeholder analysis for a maternal and newborn health project in Eastern Uganda. BMC Pregnancy and Childbirth, 13(58), 1–12. https://doi.org/10.1186/1471-2393-13-58
Nolna, S. K., Bonono, C. R., Moncher, M. N., Bindé, T., Nolna, D., & Zogo, P. O. (2018). Factors influencing the performance of routine immunization in urban areas: A comparative case study of two cities in Cameroon: Douala and Yaoundé. Vaccine, 36(49), 7549–7555. https://doi.org/10.1016/j.vaccine.2018.10.048
Noviyanti, Gamaputra, G., Lestari, Y., & Utami, D. A. (2018). Pengidentifikasian Pendapatan dan Prioritas Penggunaan Dana Desa. PUBLISIA:Jurnal Ilmu Administrasi Publik, 3(2), 112–121.
Purbani, R. K., Mahendradhata, Y., & Subronto, Y. W. (2019). Analisis Stakeholder dalam Penanggulangan HIV-AIDS di Kabupaten Grobogan. Jurnal Kebijakan Kesehatan Indonesia, 08(03), 136–141. https://jurnal.ugm.ac.id/jkki/article/view/37538
Sari, W., & Nadjib, M. (2019). Determinan Cakupan Imunisasi Dasar Lengkap pada Penerima Program Keluarga Harapan. Jurnal Ekonomi Kesehatan Indonesia, 4(1), 1–9. https://doi.org/10.7454/eki.v4i1.3087
Sell, H., Assi, A., Driedger, S. M., Dubé, È., Gagneur, A., Meyer, S. B., Robinson, J., Sadarangani, M., Tunis, M., & MacDonald, S. E. (2021). Continuity of routine immunization programs in Canada during the COVID-19 pandemic. Vaccine, 39(39), 5532–5537. https://doi.org/10.1016/j.vaccine.2021.08.044
Senewe, M. S., Rompas, S., & Lolong, J. (2017). Analisis Faktor-Faktor yang Berhubungan dengan Kepatuhan Ibu dalam Pemberian Imunisasi Dasar di Puskesmas Tongkaina Kecamatan Bunaken Kotamadya Manado. Jurnal Keperawatan, 5(1), 1–12. https://ejournal.unsrat.ac.id/index.php/jkp/article/view/14732
Singh, S., Sahu, D., Agrawal, A., & Vashi, M. D. (2019). Barriers and opportunities for improving childhood immunization coverage in slums: A qualitative study. Preventive Medicine Reports, 14(March), 100858. https://doi.org/10.1016/j.pmedr.2019.100858
Sriatmi, A., Jati, S. P., Suryoputro, A., & Fatmasari, E. Y. (2021). Stakeholder Mapping Analysis on the Scaling-Up Nutrition Movement during the 1000 Days of Life between the Urban and Rural Government Areas. Unnes Journal of Public Health, 10(1), 68–77. https://doi.org/10.15294/ujph.v10i1.38029
Triana, V. (2016). Faktor yang Berhubungan dengan Pemberian Imunisasi Dasar Lengkap pada Bayi Tahun 2015. Jurnal Kesehatan Masyarakat Andalas, 10(2), 123–135. http://jurnal.fkm.unand.ac.id/index.php/jkma/article/view/196/182
Copyright (c) 2022 Ayun Sriatmi, Sutopo Patria Jati, Wulan Kusumastuti

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
Authors retain copyright and grant the journal right of first publication with the work simultaneously licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License that allows others to share the work with an acknowledgment of the work's authorship and initial publication in this journal.
Authors are able to enter into separate, additional contractual arrangements for the non-exclusive distribution of the journal's published version of the work (e.g., post it to an institutional repository or publish it in a book), with an acknowledgment of its initial publication in this journal.
Authors are permitted to publish their work online in third parties as it can lead to wider dissemination of the work.






