Social Vulnerability towards Covid-19 Cases in Palembang City: A Spatial Analysis in Indonesia
Abstract
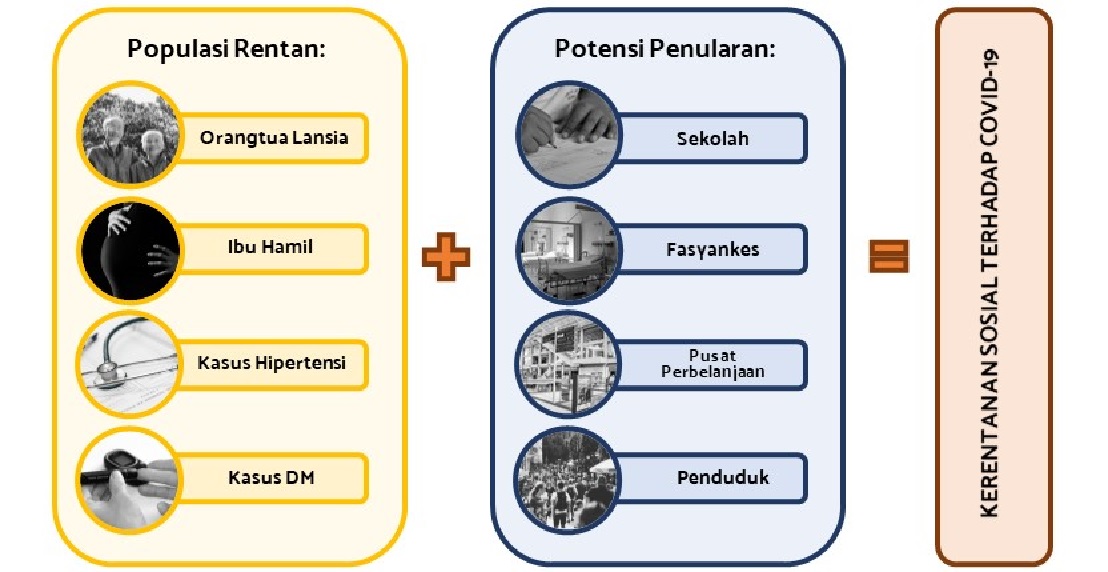
Social vulnerability is defined as a characteristic of groups that can threaten their ability to prevent, cope with or recover from the impact of a hazard. By linking social conditions with risk exposure, social vulnerability is useful for looking at the inequality of the social effects experienced by society from health crises such as the Covid-19 pandemic. The purpose of this study was to spatially analyze the vulnerability to Covid-19 in the Palembang City sub-district in 2021 by using the social characteristics of the region. This type of research was descriptive with an ecological study design. The population group studied was 18 sub-districts in the city of Palembang. The study used secondary data such as the Covid-19 variable and the vulnerable population received from the Palembang City Health Office, and the rest of the variable from the government's official website and Google Maps. The analysis process was done through Spatial Multi-Criteria Evaluation (SMCE) using Microsoft Excel and spatial analysis in weighted overlays using QGIS. For the final social vulnerability status, sub-districts with high vulnerability were Sukarami, Ilir Barat I, Plaju, and Ilir Timur I, respectively. For sub-districts with low vulnerability were Bukit Kecil and Sematang Borang. One way to reduce the level of vulnerability in an area was by taking preventive measures in the community whose needs needed to be further considered and maximizing the implementation of 3T activities and vaccinations.
Downloads
References
Abdelbadee, A. Y., & Abbas, A. M. (2020). Impact of COVID-19 on reproductive health and maternity services in low resource countries. European Journal of Contraception and Reproductive Health Care, 25(5), 402–404. https://doi.org/10.1080/13625187.2020.1768527
Akgor, U., Fadıloglu, E., Soyak, B., Unal, C., Cagan, M., Temiz, B. E., Erzenoglu, B. E., Ak, S., Gultekin, M., & Ozyuncu, O. (2021). Anxiety, depression and concerns of pregnant women during the COVID-19 pandemic. Archives of Gynecology and Obstetrics, 304(1), 125–130. https://doi.org/10.1007/s00404-020-05944-1
Alshogran, O. Y., Altawalbeh, S. M., Al-Azzam, S. I., & Karasneh, R. (2021). Predictors of Covid-19 case fatality rate: An ecological study. Annals of Medicine and Surgery, 65(April), 102319. https://doi.org/10.1016/j.amsu.2021.102319
Araújo, M. P. D., de Araújo Nunes, V. M., de Albuquerque Costa, L., de Souza, T. A., de Vasconcelos Torres, G., & Nobre, T. T. X. (2021). Health conditions of potential risk for severe Covid-19 in institutionalized elderly people. PLoS ONE, 16(1 January), 1–10. https://doi.org/10.1371/journal.pone.0245432
Bamweyana, I., Okello, D. A., Ssengendo, R., Mazimwe, A., Ojirot, P., Mubiru, F., Ndungo, L., Kiyingi, C. N., Ndyabakira, A., Bamweyana, S., & Zabali, F. (2020). Socio-Economic Vulnerability to COVID-19: The Spatial Case of Greater Kampala Metropolitan Area (GKMA). Journal of Geographic Information System, 12(04), 302–318. https://doi.org/10.4236/jgis.2020.124019
Bhadra, A., Mukherjee, A., & Sarkar, K. (2021). Impact of population density on Covid-19 infected and mortality rate in India. Modeling Earth Systems and Environment, 7(1), 623–629. https://doi.org/10.1007/s40808-020-00984-7
Birkmann, J., Cardona, O. D., Carreño, M. L., Barbat, A. H., Pelling, M., Schneiderbauer, S., Kienberger, S., Keiler, M., Alexander, D., Zeil, P., & Welle, T. (2013). Framing vulnerability, risk and societal responses: The MOVE framework. Natural Hazards, 67(2), 193–211. https://doi.org/10.1007/s11069-013-0558-5
Cai, J., Sun, W., Huang, J., Gamber, M., Wu, J., & He, G. (2020). Indirect virus transmission in cluster of COVID-19 cases, Wenzhou, China, 2020. Emerging Infectious Diseases, 26(6), 1343–1345. https://doi.org/10.3201/EID2606.200412
De Araújo Morais, A. H., Aquino, J. D. S., Da Silva-Maia, J. K., Vale, S. H. D. L., MacIel, B. L. L., & Passos, T. S. (2021). Nutritional status, diet and viral respiratory infections: Perspectives for severe acute respiratory syndrome coronavirus 2. British Journal of Nutrition, 125(8), 851–862. https://doi.org/10.1017/S0007114520003311
De Souza, C. D. F., Machado, M. F., & Do Carmo, R. F. (2020). Human development, social vulnerability and COVID-19 in Brazil: A study of the social determinants of health. Infectious Diseases of Poverty, 9(1), 4–13. https://doi.org/10.1186/s40249-020-00743-x
Delmelle, E., & Kanaroglou, P. S. (2016). Introduction: Spatial analysis and health. Spatial Analysis in Health Geography, 1, 1–12. https://doi.org/10.4324/9781315610252
Dinas Kesehatan Kota Palembang. (2021). Laporan Situasi Covid-19 Kota palembang – March 29th 2021. In Situasi COVID-19 Kota Palembang (Issue Maret).
Dinas Kesehatan Kota Palembang. (2022). Berita : Booster Vaksinasi COVID-19 - Dinas Kesehatan Kota Palembang. Dinas Kesehatan Kota Palembang. https://dinkes.palembang.go.id/?nmodul=berita&bhsnyo=id&bid=1652
Dinas Kesehatan Provinsi Sumatera Selatan. (2021). Update Covid-19 Sumsel 30 Maret 2021 - Situasi Terkini Perkembangan Covid-19 Prov. Sumsel. http://corona.sumselprov.go.id/index.php?module=dataterkinidetail&id=419
Dinas Kominfo Kota Palembang. (2021). Pemkot Mulai Vaksinasi Petugas Pelayanan Publik dan Lansia. Pemerintah Kota Palembang. https://palembang.go.id/pemkot_mulai_vaksinasi_petugas_pelayanan_publik_dan_lansia
Doyle, T., Kendrick, K., Troelstrup, T., Gumke, M., Edwards, J., Chapman, S., Propper, R., Rivkees, S. A., & Blackmore, C. (2021). COVID-19 in Primary and Secondary School Settings During the First Semester of School Reopening — Florida, August-December 2020. MMWR Surveillance Summaries, 70(12), 437–441. https://doi.org/10.15585/mmwr.mm7012e2
Fatima, M., O’keefe, K. J., Wei, W., Arshad, S., & Gruebner, O. (2021). Geospatial analysis of covid-19: A scoping review. International Journal of Environmental Research and Public Health, 18(5), 1–14. https://doi.org/10.3390/ijerph18052336
Gazzaz, Z. J. (2021). Diabetes and COVID-19. Open Life Sciences, 16(1), 297–302. https://doi.org/10.1515/biol-2021-0034
Hammad, O. A., Alnazzawi, A., Borzangy, S. S., Abu-Hammad, A., Fayad, M., Saadaledin, S., Abu-Hammad, S., & Odeh, N. D. (2020). Factors influencing global variations in covid-19 cases and fatalities; a review. Healthcare (Switzerland), 8(3). https://doi.org/10.3390/healthcare8030216
Januraga, P. P., & Harjana, N. P. A. (2020). Improving Public Access to COVID-19 Pandemic Data in Indonesia for Better Public Health Response. Frontiers in Public Health, 8, 825. https://doi.org/10.3389/fpubh.2020.563150
Kandel, N., Chungong, S., Omaar, A., & Xing, J. (2020). Health security capacities in the context of COVID-19 outbreak: an analysis of International Health Regulations annual report data from 182 countries. The Lancet, 395(10229), 1047–1053. https://doi.org/10.1016/S0140-6736(20)30553-5
Kanga, S., Meraj, G., Sudhanshu, Farooq, M., Nathawat, M. S., & Singh, S. K. (2021). Analyzing the Risk to COVID-19 Infection using Remote Sensing and GIS. Risk Analysis, 41(5), 801–813. https://doi.org/10.1111/risa.13724
Kementerian Kesehatan RI. (2021a). Program Vaksinasi COVID-19 Mulai Dilakukan, Presiden Orang Pertama Penerima Suntikan Vaksin COVID-19. Direktorat Jenderal Pencegahan Dan Pengendalian Penyakit, Kementerian Kesehatan Republik Indonesia. http://p2p.kemkes.go.id/program-vaksinasi-covid-19-mulai-dilakukan-presiden-orang-pertama-penerima-suntikan-vaksin-covid-19/
Kementerian Kesehatan RI. (2021b). Situasi Terkini Perkembangan Coronavirus Disease (COVID-19) – March 29th 2021. The Ministry of Health of The Republic of Indonesia. https://infeksiemerging.kemkes.go.id/situasi-infeksi-emerging/situasi-terkini-perkembangan-coronavirus-disease-covid-19-29-maret-2021
Kim, S. J., & Bostwick, W. (2020). Social Vulnerability and Racial Inequality in COVID-19 Deaths in Chicago. Health Education and Behavior, 47(4), 509–513. https://doi.org/10.1177/1090198120929677
Kok, D. Q. R., & Woo, W. T. (2021). Saving lives and livelihoods in the covid-19 pandemic: What have we learned, particularly from asia? Asian Economic Papers, 20(1), 1–29. https://doi.org/10.1162/asep_a_00833
Li, G., Liu, Y., Jing, X., Wang, Y., Miao, M., Tao, L., Zhou, Z., Xie, Y., Huang, Y., Jianhua, L., Guozhong, G., Jin, P., Hao, Y., Faria, N. R., De Clercq, E., & Zhang, M. (2021). Mortality risk of COVID-19 in elderly males with comorbidities: a multi-country study. Aging, 13(1), 27–60. https://doi.org/10.18632/aging.202456
Lim, S., Bae, J. H., Kwon, H. S., & Nauck, M. A. (2021). COVID-19 and diabetes mellitus: from pathophysiology to clinical management. Nature Reviews Endocrinology, 17(1), 11–30. https://doi.org/10.1038/s41574-020-00435-4
Mas’udi, W., & Winanti, P. S. (2020). Tata Kelola Penanganan Covid-19 Di Indonesia: Kajian Awal (W. Mas’udi & P. S. Winanti (eds.)). Gadjah Mada University Press.
Nayak, A., Islam, S. J., Mehta, A., Ko, Y. A., Patel, S. A., Goyal, A., Sullivan, S., Lewis, T. T., Vaccarino, V., Morris, A. A., & Quyyumi, A. A. (2020). Impact of Social Vulnerability on COVID-19 Incidence and Outcomes in the United States. MedRxiv, 1–27. https://doi.org/10.1101/2020.04.10.20060962
Neelon, B., Mutiso, F., Mueller, N. T., Pearce, J. L., & Benjamin-Neelon, S. E. (2021). Spatial and temporal trends in social vulnerability and COVID-19 incidence and death rates in the United States. PLoS ONE, 16(3 March), 1–17. https://doi.org/10.1371/journal.pone.0248702
Nsanzabera, C. (2021). Health Promotion to Reduce Hypertension Patients’ Vulnerability to Coronavirus Disease-19 (COVID-19). International Journal of Cardiovascular Sciences, 34(1), 99–102. https://doi.org/10.36660/ijcs.20200147
Pan, L., Wang, J., Wang, X., Ji, J. S., Ye, D., Shen, J., Li, L., Liu, H., Zhang, L., Shi, X., & Wang, L. (2021). Prevention and control of coronavirus disease 2019 (COVID-19) in public places. In Environmental Pollution (Vol. 292, Issue June 2020). https://doi.org/10.1016/j.envpol.2021.118273
Roy, S., Bhunia, G. S., & Shit, P. K. (2021). Spatial prediction of COVID-19 epidemic using ARIMA techniques in India. Modeling Earth Systems and Environment, 7(2), 1385–1391. https://doi.org/10.1007/s40808-020-00890-y
Satuan Tugas Penanganan COVID-19. (2022). Capaian Vaksinasi Covid-19 Indonesia Naik ke Peringkat Empat Dunia | Covid19.go.id. Satuan Tugas Penanganan COVID-19. https://covid19.go.id/artikel/2022/01/10/capaian-vaksinasi-covid-19-indonesia-naik-ke-peringkat-empat-dunia
Siegel, R. M., & Mallow, P. J. (2021). The Impact of COVID-19 on Vulnerable Populations and Implications for Children and Health Care Policy. Clinical Pediatrics, 60(2), 93–98. https://doi.org/10.1177/0009922820973018
Sun, H., Ning, R., Tao, Y., Yu, C., Deng, X., Zhao, C., Meng, S., Tang, F., & Xu, D. (2020). Risk Factors for Mortality in 244 Older Adults With COVID-19 in Wuhan, China: A Retrospective Study. Journal of the American Geriatrics Society, 68(6), E19–E23. https://doi.org/10.1111/jgs.16533
Wang, J., Zhou, M., & Liu, F. (2020). Reasons for healthcare workers becoming infected with novel coronavirus disease 2019 (COVID-19) in China. In Journal of Hospital Infection (Vol. 105, Issue 1, pp. 100–101). W.B. Saunders Ltd. https://doi.org/10.1016/j.jhin.2020.03.002
WHO. (2021). Coronavirus disease (COVID-19): Variants of SARS-COV-2. Word Health Organization. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/question-and-answers-hub/q-a-detail/coronavirus-disease-%28covid-19%29-variants-of-sars-cov-2?gclid=Cj0KCQiA_8OPBhDtARIsAKQu0gaVxS4Fqppu2VhYQAI13SWLzhNAEMX5tHrtiJ5FXfUdUoy4NG3quuwaApOiEALw_wc
Wong, D. W. S., & Li, Y. (2020). Spreading of COVID-19: Density matters. PLoS ONE, 15(12 December), 1–16. https://doi.org/10.1371/journal.pone.0242398
World Health Organization. (2021). COVID-19 Weekly Epidemiological Update - 30 March 2021. In World Health Organization (Issue December). https://www.who.int/docs/default-source/coronaviruse/situation-reports/weekly_epidemiological_update_22.pdf
Xie, Z., Qin, Y., Li, Y., Shen, W., Zheng, Z., & Liu, S. (2020). Spatial and temporal differentiation of COVID-19 epidemic spread in mainland China and its influencing factors. Science of the Total Environment, 744, 140929. https://doi.org/10.1016/j.scitotenv.2020.140929
Zhao, P., Zhang, N., & Li, Y. (2020). A comparison of infection venues of COVID-19 case clusters in northeast China. International Journal of Environmental Research and Public Health, 17(11), 1–14. https://doi.org/10.3390/ijerph17113955
Copyright (c) 2022 Marisa Nurhaliza, Amrina Rosada

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
Authors retain copyright and grant the journal right of first publication with the work simultaneously licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License that allows others to share the work with an acknowledgment of the work's authorship and initial publication in this journal.
Authors are able to enter into separate, additional contractual arrangements for the non-exclusive distribution of the journal's published version of the work (e.g., post it to an institutional repository or publish it in a book), with an acknowledgment of its initial publication in this journal.
Authors are permitted to publish their work online in third parties as it can lead to wider dissemination of the work.