Effect of Birth Interval Upon Neonatal Deaths in Indonesia: 5-Year-Based Calendar Data
Abstract
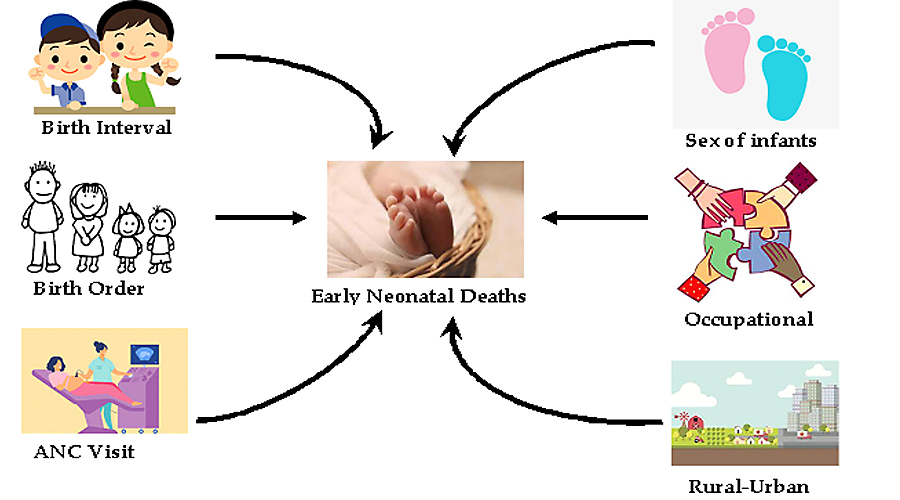
Early neonatal deaths, defined as deaths of newborn babies between zero and seven days, have undoubtedly triggered a big challenge in developing countries. This current analysis aimed to determine the effect of birth interval (i.e., the time between two successive live births) on adverse pregnancy outcomes such as early neonatal death by using reproductive calendar data containing information on birth history for five years preceding Indonesia Demographic and Health Survey 2017. Merely singleton and non-first live births were included in the analysis (n=11, 599). Logistic regression models for the complex sample were utilized to measure the associations between birth interval and early neonatal deaths after adjusting for potential confounders. Early neonatal mortality was associated with birth interval. Newborns with shorter birth intervals (< 24 months) and longer birth intervals (36 months or more) had 2.68 times (95% CI: 1.15-6.28) and 3.08 times (95% CI: 1.37-6.92), respectively, higher odds of early neonatal deaths compared with newborns birth spaced of 24-35 months. Among mothers who received at least one antenatal care visit, there was a decrease in the odds of early neonatal deaths for shorter and longer birth intervals. The results suggest that the promotion of optimal birth interval, the utilization of antenatal care services, and the improvement of contraceptive services are all important to prevent adverse pregnancy outcomes.
Downloads
References
Afeworki, R., Smits, J., Tolboom, J., & van der Ven, A. (2015). Positive effect of large birth intervals on early childhood hemoglobin levels in Africa is limited to girls: cross-sectional DHS study. PLoS ONE, 10(6), 1–14. https://doi.org/10.1371/journal.pone.0131897
Aghai, Z. H., Goudar, S. S., Patel, A., Saleem, S., Dhaded, S. M., Kavi, A., Lalakia, P., Naqvi, F., Hibberd, P. L., McClure, E. M., Nolen, T. L., Iyer, P., Goldenberg, R. L., & Derman, R. J. (2020). Gender variations in neonatal and early infant mortality in India and Pakistan: a secondary analysis from the Global Network Maternal Newborn Health Registry. Reproductive Health, 17(3), 1–12. https://doi.org/10.1186/s12978-020-01028-0
Ahrens, K. A., Nelson, H., Stidd, R. L., Moskosky, S., & Hutcheon, J. A. (2019). Short interpregnancy intervals and adverse perinatal outcomes in high-resource settings: An updated systematic review. Paediatric and Perinatal Epidemiology, 33(1), O25–O47. https://doi.org/10.1111/ppe.12503
Chungkham, H. S., Sahoo, H., & Marbaniang, S. P. (2020). Birth interval and childhood undernutrition: Evidence from a large scale survey in India. Clinical Epidemiology and Global Health, 8(4), 1189–1194. https://doi.org/10.1016/j.cegh.2020.04.012
Conde-Agudelo, A., Rosas-Bermudez, A., Castaño, F., & Norton, M. H. (2012). Effects of Birth Spacing on Maternal, Perinatal, Infant, and Child Health: A Systematic Review of Causal Mechanisms. Studies in Family Planning, 43(2), 93–114. https://doi.org/10.1111/j.1728-4465.2012.00308.x
Dhingra, S., & Pingali, P. L. (2021). Effects of short birth spacing on birth-order differences in child stunting: Evidence from India. Proceedings of the National Academy of Sciences of the United States of America, 118(8), 1–8. https://doi.org/10.1073/pnas.2017834118
Duclos, D., Cavallaro, F. L., Ndoye, T., Faye, S. L., Diallo, I., Lynch, C. A., Diallo, M., Faye, A., & Penn-Kekana, L. (2019). Critical insights on the demographic concept of “birth spacing”: locating Nef in family well-being, bodies, and relationships in Senegal. Sexual and Reproductive Health Matters, 27(1), 136–145. https://doi.org/10.1080/26410397.2019.1581533
Ezeh, O. K., Uche-Nwachi, E. O., Abada, U. D., & Agho, K. E. (2019). Community-and proximate-level factors associated with perinatal mortality in Nigeria: Evidence from a nationwide household survey. BMC Public Health, 19(1), 1–9. https://doi.org/10.1186/s12889-019-7151-0
Fotso, J. C., Cleland, J., Mberu, B., Mutua, M., & Elungata, P. (2013). Birth spacing and child mortality: An analysis of prospective data from the nairobi urban health and demographic surveillance system. Journal of Biosocial Science, 45, 779–798. https://doi.org/10.1017/S0021932012000570
Ghimire, P. R., Agho, K. E., Renzaho, A. M. N., Nisha, M. K., Dibley, M., & Raynes-Greenow, C. (2019). Factors associated with perinatal mortality in Nepal: Evidence from Nepal demographic and health survey 2001-2016. BMC Pregnancy and Childbirth, 19(1), 1–12. https://doi.org/10.1186/s12884-019-2234-6
Hailu, D., & Gulte, T. (2016). Determinants of Short Interbirth Interval among Reproductive Age Mothers in Arba Minch District, Ethiopia. International Journal of Reproductive Medicine, 1–17. https://doi.org/10.1155/2016/6072437
Hatt, L., Stanton, C., Ronsmans, C., Makowiecka, K., & Adisasmita, A. (2009). Did professional attendance at home births improve early neonatal survival in Indonesia. Health Policy and Planning, 24(4), 270–278. https://doi.org/10.1093/heapol/czp012
Hossain, M. B., Mistry, S. K., Mohsin, M., & Khan, M. H. R. (2019). Trends and determinants of perinatal mortality in Bangladesh. PLoS ONE, 14(8), 1–19. https://doi.org/10.1371/journal.pone.0221503
Jena, B. H., Biks, G. A., Gelaye, K. A., & Gete, Y. K. (2020). Magnitude and trend of perinatal mortality and its relationship with inter-pregnancy interval in Ethiopia: A systematic review and meta-analysis. BMC Pregnancy and Childbirth, 20(1), 1–13. https://doi.org/10.1186/s12884-020-03089-2
Kannaujiya, A. K., Kumar, K., Upadhyay, A. K., McDougal, L., Raj, A., & Singh, A. (2020). Short interpregnancy interval and low birth weight births in India: Evidence from National Family Health Survey 2015-16. SSM-Population Health, 12, 100700. https://doi.org/10.1016/j.ssmph.2020.100700
Kibria, G. M. Al, Burrowes, V., Choudhury, A., Sharmeen, A., Ghosh, S., Mahmud, A., & Angela, K. C. (2018). Determinants of early neonatal mortality in Afghanistan: An analysis of the Demographic and Health Survey 2015. Globalization and Health, 14(1), 1–12. https://doi.org/10.1186/s12992-018-0363-8
Lawn, J. E., Blencowe, H., Oza, S., You, D., Lee, A. C. C., Waiswa, P., Lalli, M., Bhutta, Z., Barros, A. J. D., Christian, P., Mathers, C., & Cousens, S. N. (2014). Every newborn: Progress, priorities, and potential beyond survival. The Lancet, 384(9938), 189–205. https://doi.org/10.1016/S0140-6736(14)60496-7
Lehtonen, L., Gimeno, A., Parra-Llorca, A., & Vento, M. (2017). Early neonatal death: A challenge worldwide. Seminars in Fetal and Neonatal Medicine, 22(3), 153–160. https://doi.org/10.1016/j.siny.2017.02.006
Liu, L., Oza, S., Hogan, D., Chu, Y., Perin, J., Zhu, J., Lawn, J. E., Cousens, S., Mathers, C., & Black, R. E. (2016). Global, regional, and national causes of under-5 mortality in 2000–15: an updated systematic analysis with implications for the Sustainable Development Goals. The Lancet, 388(10063), 3027–3035. https://doi.org/10.1016/S0140-6736(16)31593-8
Migoto, M. T., Oliveira, R. P. de, Silva, A. M. R., & Freire, M. H. de S. (2018). Early neonatal mortality and risk factors: a case-control study in Paraná State. Revista Brasileira de Enfermagem, 71(5), 2527–2534. https://doi.org/10.1590/0034-7167-2016-0586
Molitoris, J. (2017). The Effect of Birth Spacing on Child Mortality in Sweden, 1878–1926. Population and Development Review, 43(1), 61–82. https://doi.org/10.1111/padr.12050
Molitoris, J. (2018). Heterogeneous Effects of Birth Spacing on Neonatal Mortality Risks in Bangladesh. Studies in Family Planning, 49(1), 3–21. https://doi.org/10.1017/s0084255900044454
Molitoris, J., Barclay, K., & Kolk, M. (2018). When birth spacing does and does not matter for child survival: an international comparison using the DHS. Stockholm Research Reports in Demography, 2018, 21. https://doi.org/10.17045/STHLMUNI.6843107.V1
National Population and Family Planning Board, Statistics Indonesia, Ministry of Health, & ICF. (2018). Indonesia Demographic and Health Survey 2017. BKKBN. https://dhsprogram.com/pubs/pdf/FR342/FR342.pdf
Nisha, M. K., Alam, A., Islam, M. T., Huda, T., & Raynes-Greenow, C. (2019). Risk of adverse pregnancy outcomes associated with short and long birth intervals in Bangladesh: Evidence from six Bangladesh Demographic and Health Surveys, 1996-2014. BMJ Open, 9(2), 1–11. https://doi.org/10.1136/bmjopen-2018-024392
Onwuka, C., Ugwu, E., Obi, S., Onwuka, C., Dim, C., Ezugwu, E., Agu, P., Nwagha, U., & Ozumba, B. (2020). Effects of Short Inter-Pregnancy Interval on Maternal and Perinatal Outcomes: A Cohort Study of Pregnant Women in a Low-Income Country. Nigerian Journal of Clinical Practice, 23, 928–933. https://doi.org/10.4103/njcp.njcp
Sankar, M. J., Neogi, S. B., Sharma, J., Chauhan, M., Srivastava, R., Prabhakar, P. K., Khera, A., Kumar, R., Zodpey, S., & Paul, V. K. (2016). State of newborn health in India. Journal of Perinatology, 36(s3), S3–S8. https://doi.org/10.1038/jp.2016.183
Subedi, S., Katz, J., Erchick, D. J., Verhulst, A., Khatry, S. K., Mullany, L. C., Tielsch, J. M., Leclerq, S. C., Christian, P., West, K. P., & Guillot, M. (2022). Does higher early neonatal mortality in boys reverse over the neonatal period? A pooled analysis from three trials of Nepal. BMJ Open, 12(5). https://doi.org/10.1136/bmjopen-2021-056112
Swaminathan, A., Fell, D. B., Regan, A., Walker, M., & Corsi, D. J. (2020). Association between interpregnancy interval and subsequent stillbirth in 58 low-income and middle-income countries: a retrospective analysis using Demographic and Health Surveys. The Lancet Global Health, 8(1), e113–e122. https://doi.org/10.1016/S2214-109X(19)30458-9
Thoma, M. E., Rossen, L. M., De Silva, D. A., Warner, M., Simon, A. E., Moskosky, S., & Ahrens, K. A. (2019). Beyond birth outcomes: Interpregnancy interval and injury-related infant mortality. Paediatric and Perinatal Epidemiology, 33(5), 360–370. https://doi.org/10.1111/ppe.12575
Thomas, M. G., Shanley, D. P., Houston, A. I., Mcnamara, J. M., Mace, R., & Kirkwood, T. B. L. (2015). A dynamic framework for the study of optimal birth intervals reveals the importance of sibling competition and mortality risks. Journal of Evolutionary Biology, 28(4), 885–895. https://doi.org/10.1111/jeb.12613
Titaley, C. R., Dibley, M. J., & Roberts, C. L. (2012). Type of delivery attendant, place of delivery and risk of early neonatal mortality: Analyses of the 1994-2007 Indonesia Demographic and Health Surveys. Health Policy and Planning, 27(5), 405–416. https://doi.org/10.1093/heapol/czr053
USAID. (2018). DHS Contraceptive Calendar Tutorial: The Demographic and Health Survey Program. https://www.dhsprogram.com/data/calendar-tutorial/
Yadeta, T. A., Mengistu, B., Gobena, T., & Regassa, L. D. (2020). Spatial pattern of perinatal mortality and its determinants in Ethiopia: Data from Ethiopian Demographic and Health Survey 2016. PLoS ONE, 15(11 November), 1–19. https://doi.org/10.1371/journal.pone.0242499
Ye, L., Cao, W., Yao, J., Peng, G., & Zhou, R. (2019). Systematic review of the effects of birth spacing after cesarean delivery on maternal and perinatal outcomes. International Journal of Gynecology and Obstetrics, 147(1), 19–28. https://doi.org/10.1002/ijgo.12895
Copyright (c) 2022 Maria Gayatri, Dian Kristiani Irawaty

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
Authors retain copyright and grant the journal right of first publication with the work simultaneously licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License that allows others to share the work with an acknowledgment of the work's authorship and initial publication in this journal.
Authors are able to enter into separate, additional contractual arrangements for the non-exclusive distribution of the journal's published version of the work (e.g., post it to an institutional repository or publish it in a book), with an acknowledgment of its initial publication in this journal.
Authors are permitted to publish their work online in third parties as it can lead to wider dissemination of the work.






