Non-Communicable Disease Morbidity Among Young Adults: A Cross-Sectional Study in Indonesia
Abstract
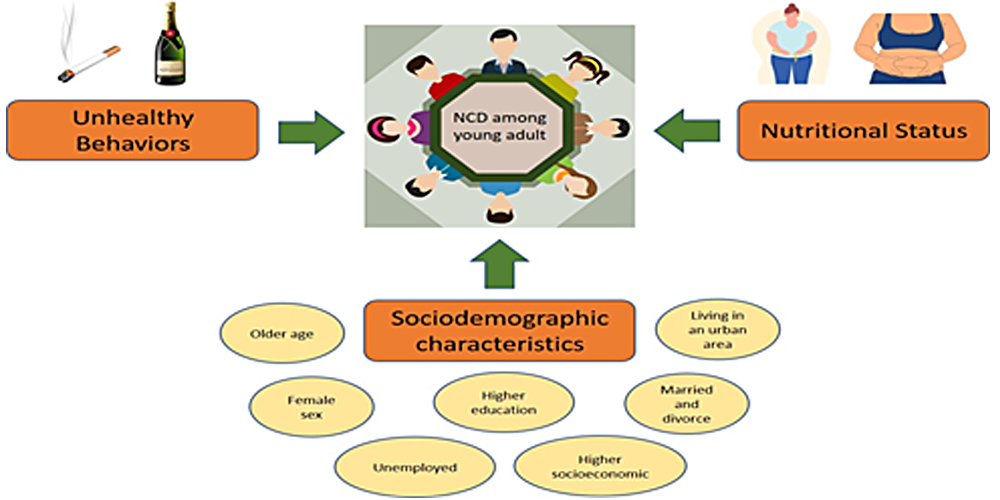
Noncommunicable Disease (NCD) has continued to pose a significant global burden, specifically regarding morbidity among young adults which has not been well studied. Therefore, this study aimed to assess the burden of NCD among young adults and identify correlating factors. It analyzed the 2018 Indonesian Basic Health Research, a nationwide study employing a cross-sectional design and linear systematic with Two Stage Sampling. The subject involved comprised 319,355 individuals in the 18-40 age group. Data were further analyzed using bivariate and multivariate analysis with logistic regression. The analysis results showed that 6% of young adults in Indonesia had one NCD or more. Young adults with higher Waist Circumference (WC) and higher Body Mass Index (BMI) had a higher risk of NCD (OR:1.58; 95%CI;1.52-1.65 and OR: 1.14; 95%CI:1.09-1.19, respectively). Furthermore, several sociodemographic factors exhibited significant correlation including older age, female sex, unemployment, higher educational and socioeconomic status, married and divorced, as well as living in an urban area (p-value<0.05). Unhealthy behavior such as consuming alcohol and smoking also increased the risk for NCD morbidity (OR:1.20; 95%CI;1.10-1.30 and OR: 1.19; 95%CI:1.10-1.27). Therefore, it was crucial to strengthen preventive programs targeting NCD among young adults by focusing on sociodemographic characteristics. This study also emphasized the importance of campaigns aimed at improving health behavior in this age group.
Downloads
References
Adegbite, B. R., Edoa, J. R., Agbo Achimi Abdul, J. B. P., Epola, M., Mevyann, C., Dejon-Agobé, J. C., Zinsou, J. F., Honkpehedji, Y. J., Mpagama, S. G., Alabi, A. S., Kremsner, P. G., Klipstein-Grobusch, K., Adegnika, A. A., & Grobusch, M. P. (2022). Non-communicable disease co-morbidity and associated factors in tuberculosis patients: A cross-sectional study in Gabon. EClinicalMedicine, 45, 101316. https://doi.org/10.1016/j.eclinm.2022.101316
Akseer, N., Mehta, S., Wigle, J., Chera, R., Brickman, Z. J., Al-Gashm, S., Sorichetti, B., Vandermorris, A., Hipgrave, D. B., Schwalbe, N., & Bhutta, Z. A. (2020). Non-communicable diseases among adolescents: current status, determinants, interventions and policies. BMC Public Health, 20(1), 1–20. https://doi.org/10.1186/s12889-020-09988-5
Alnakhi, W. K., Mamdouh, H., Hussain, H. Y., Ibrahim, G. M., Ahmad, A. S., Ali, R., & Abdulle, A. (2021). The socio-demographic characteristics associated with non-communicable diseases among the adult population of dubai: Results from dubai household survey 2019. Healthcare (Switzerland), 9(9). https://doi.org/10.3390/healthcare9091139
Asogwa, O. A., Boateng, D., Marzà-Florensa, A., Peters, S., Levitt, N., Van Olmen, J., & Klipstein-Grobusch, K. (2022). Multimorbidity of non-communicable diseases in low-income and middle-income countries: a systematic review and meta-analysis. BMJ Open, 12(1), e049133. https://doi.org/10.1136/BMJOPEN-2021-049133
Ayodapo, A., & Ibisola, B. (2021). Smoking and Non-Communicable Diseases in Sub-Saharan Africa: The Nigeria Scenario. In Lifestyle and Epidemiology - Poverty and Cardiovascular Diseases a Double Burden in African Populations [Working Title]. IntechOpen. https://doi.org/10.5772/intechopen.96693
Bhatt, G., Goel, S., Grover, S., Kaur, N., & Singh, S. (2021). A cross sectional study to assess tobacco use and its correlates among patients attending non‑communicable disease clinics of a Northern Jurisdiction in India Garima. Journal of Family Medicine and Primary Care, 10(8), 2915–2922. https://doi.org/10.4103/jfmpc.jfmpc
Bista, B., Dhungana, R. R., Chalise, B., & Pandey, A. R. (2020). Prevalence and determinants of noncommunicable diseases risk factors among reproductive aged women of Nepal: Results from Nepal demographic Health Survey 2016. PLoS ONE, 15(3), 1–13. https://doi.org/10.1371/journal.pone.0218840
Biswas, T., Townsend, N., Islam, M. S., Islam, M. R., Das Gupta, R., Das, S. K., & Mamun, A. Al. (2019). Association between socioeconomic status and prevalence of non-communicable diseases risk factors and comorbidities in Bangladesh: findings from a nationwide cross-sectional survey. BMJ Open, 9(3), e025538. https://doi.org/10.1136/bmjopen-2018-025538
Bonnie, R., Brindis, C., Carrion, G., Courtney, M., Crosnose, Ro., Davis, M., Harris, K. M., Holzer, H., Irwin, C., Luna, B., Murry, V. M., Papacharissi, Z., Schulenberg, J., Sepulveda, M., Viswanath, K., & Walker, L. (2015). Young Adults and Public Health. In Institute of Medicine and National Research Council of The National Academies. https://nap.nationalacademies.org/resource/18869/YAs_Public_Health_Brief.pdf
Bramhankar, M., Pandey, M., Rana, G. S., Rai, B., Mishra, N. L., & Shukla, A. (2021). An assessment of anthropometric indices and its association with NCDs among the older adults of India: evidence from LASI Wave-1. BMC Public Health, 21(1), 1–13. https://doi.org/10.1186/s12889-021-11421-4
Brennan, L., Klassen, K., Weng, E., Chin, S., Molenaar, A., Reid, M., Truby, H., & McCaffrey, T. A. (2020). A social marketing perspective of young adults’ concepts of eating for health: is it a question of morality? International Journal of Behavioral Nutrition and Physical Activity, 17(1), 44. https://doi.org/10.1186/s12966-020-00946-3
Camacho, P. A., Gomez-Arbelaez, D., Otero, J., González-Gómez, S., Molina, D. I., Sanchez, G., Arcos, E., Narvaez, C., García, H., Pérez, M., Hernandez-Triana, E., Duran, M., Cure, C., Sotomayor, A., Rico, A., Cotes, F., Rangarajan, S., Yusuf, S., & López-Jaramillo, P. (2020). Self-Reported Prevalence of Chronic Non-Communicable Diseases in Relation to Socioeconomic and Educational Factors in Colombia: A Community-Based Study in 11 Departments. Global Heart, 15(1). https://doi.org/10.5334/gh.792
Charalampous, P., Gorasso, V., Plass, D., Pires, S. M., Von Der Lippe, E., Mereke, A., Idavain, J., Kissimova-Skarbek, K., Morgado, J. N., Ngwa, C. H., Noguer, I., Padron-Monedero, A., Santi-Cano, M. J., Sarmiento, R., Devleesschauwer, B., Haagsma, J. A., Ádám, B., Alkerwi, A., Bikbov, B., & Wyper, G. M. A. (2022). Burden of non-communicable disease studies in Europe: a systematic review of data sources and methodological choices. European Journal of Public Health, 32(2), 289–296. https://doi.org/10.1093/EURPUB/CKAB218
De-Wet-Billings, N., & Frade, S. (2022). Non Communicable Disease Comorbidities (NCDCs) Among Youth in South Africa: The Causal Contribution of Not Being in School or Work and Other Socioeconomic Characteristics. Journal of Public Health, 30, 1205–1212. https://doi.org/https://doi.org/10.1007/s10389-020-01398-6
Demilew, Y. M., & Firew, B. S. (2019). Factors associated with noncommunicable disease among adults in Mecha district, Ethiopia: A case control study. PLoS ONE, 14(5), 1–13. https://doi.org/10.1371/journal.pone.0216446
Dhawan, D., & Sharma, S. (2020). Abdominal Obesity, Adipokines and Non-communicable Diseases. The Journal of Steroid Biochemistry and Molecular Biology, 203, 105737. https://doi.org/10.1016/j.jsbmb.2020.105737
Effendi, D. E., Nugroho, A. P., Handayani, S., Novita, R., Purwoko, S., & Agustina, Z. A. (2022). Tobacco Consumption Among Young Population in Rural Indonesia: Prevalence and Associated Factors. Open Access Macedonian Journal of Medical Sciences, 10(E), 1178–1183. https://doi.org/10.3889/oamjms.2022.10011
Hauerslev, M., & Allen, L. (2018). Young people and noncommunicable diseases - vulnerable to disease, vital for change. International Journal of Noncommunicable Disease, 3, 45–48. https://doi.org/10.4103/jncd.jncd
Hinton, T. C., Adams, Z. H., Baker, R. P., Hope, K. A., Paton, J. F. R., Hart, E. C., & Nightingale, A. K. (2020). Investigation and treatment of high blood pressure in young people: too much medicine or appropriate risk reduction? Hypertension, 75(1), 16–22. https://doi.org/10.1161/HYPERTENSIONAHA.119.13820
Htet, A. S., Bjertness, M. B., Sherpa, L. Y., Kjøllesdal, M. K., Oo, W. M., Meyer, H. E., Stigum, H., & Bjertness, E. (2016). Urban-rural differences in the prevalence of non-communicable diseases risk factors among 25-74 years old citizens in Yangon Region, Myanmar: A cross sectional study. BMC Public Health, 16(1), 1–12. https://doi.org/10.1186/s12889-016-3882-3
Hui, L. (2017). Assessment of the role of ageing and non-ageing factors in death from non-communicable diseases based on a cumulative frequency model. Scientific Reports 2017 7:1, 7(1), 1–7. https://doi.org/10.1038/s41598-017-08539-0
Hurlock, E. B. (1999). Developmental Psychology: A life Span Approach (5th ed.). McGraw-Hill.
Joshi, V., Joshi, N. K., Suthar, P., & Jain, Y. K. (2021). Non-communicable diseases risk factors among government school teachers in Jodhpur, Rajasthan. International Journal of Public Health Science, 10(4), 920–926. https://doi.org/10.11591/IJPHS.V10I4.20895
Jung, S. O., Son, Y. H., & Choi, E. (2022). E-health literacy in older adults: an evolutionary concept analysis. BMC Medical Informatics and Decision Making, 22(1), 28. https://doi.org/10.1186/s12911-022-01761-5
Kaur, H., & Aeri, B. T. (2019). Protective impact of Ffruits and vegetable intake on cardiovascular risk factors-a review. Journal of Clinical and Diagnostic Research, 13(5), 6–9. https://doi.org/10.7860/jcdr/2019/41330.12884
Kayaroganam, R., Sarkar, S., Satheesh, S., Tamilmani, S., Sivanantham, P., & Kar, S. S. (2022). Profile of noncommunicable Disease Risk Factors Among Nurses in a Tertiary Care Hospital in South India. Asian Nursing Research, August, 1–8. https://doi.org/10.1016/j.anr.2022.07.001
Kementerian Kesehatan Republik Indonesia. (2019). Laporan Nasional Riskesdas 2018. Penerbit Balitbangkes.
Khorrami, Z., Rezapour, M., Etemad, K., Yarahmadi, S., Khodakarim, S., Mahdavi Hezaveh, A., Kameli, M., & Khanjani, N. (2020). The patterns of Non-communicable disease Multimorbidity in Iran: A Multilevel Analysis. Scientific Reports 2020 10:1, 10(1), 1–11. https://doi.org/10.1038/s41598-020-59668-y
Kwon, S. H., Myong, J.-P., Kim, H.-A., & Kim, K. Y. (2020). Association between morbidity of non-communicable disease and employment status: a comparison between Korea and the United States. BMC Public Health, 20(1), 763. https://doi.org/10.1186/s12889-020-08883-3
Lemme, B. (1995). Development in adulthood (2nd ed.). McGraw-Hill.
Malecki, S. L., Van Mil, S., Graffi, J., Breetvelt, E., Corral, M., Boot, E., Chow, E. W. C., Sanches, M., Verma, A. A., & Bassett, A. S. (2020). A genetic model for multimorbidity in young adults. Genetics in Medicine, 22(1), 132–141. https://doi.org/10.1038/s41436-019-0603-1
Marthias, T., Anindya, K., Ng, N., McPake, B., Atun, R., Arfyanto, H., Hulse, E. S. G., Zhao, Y., Jusril, H., Pan, T., Ishida, M., & Lee, J. T. (2021). Impact of non-communicable disease multimorbidity on health service use, catastrophic health expenditure and productivity loss in Indonesia: A population-based panel data analysis study. BMJ Open, 11(2), 1–13. https://doi.org/10.1136/bmjopen-2020-041870
Mishra, V. K., Srivastava, S., Muhammad, T., & Murthy, P. V. (2022). Relationship between tobacco use, alcohol consumption and non-communicable diseases among women in India: evidence from National Family Health Survey-2015-16. BMC Public Health, 22(1), 1–12. https://doi.org/10.1186/s12889-022-13191-z
Motuma, A., Regassa, L. D., Gobena, T., Roba, K. T., Berhane, Y., & Worku, A. (2022). Almost all working adults have at least one risk factor for non-communicable diseases: Survey of working adults in Eastern Ethiopia. PLOS ONE, 17(2), e0264698. https://doi.org/10.1371/JOURNAL.PONE.0264698
Mridha, M., Hasan, M., Khan, S., Hossain, M., & Sutradhar, I. (2019). Women are more vulnerable to non-communicable diseases in rural and urban Bangladesh. Current Developments in Nutrition, 3(Supplement_1). https://doi.org/10.1093/cdn/nzz039.p18-082-19
Olawuyi, A. T., & Adeoye, I. A. (2018). The prevalence and associated factors of non-communicable disease risk factors among civil servants in Ibadan, Nigeria. PLOS ONE, 13(9), e0203587. https://doi.org/10.1371/journal.pone.0203587
Pan American Health Organization. (2022). Non-communicable diseases and gender. Pan American Health Organization. https://www.paho.org/hq/dmdocuments/2011/gdr-ncd-gender-factsheet-final.pdf
Peters, R., Ee, N., Peters, J., Beckett, N., Booth, A., Rockwood, K., & Anstey, K. J. (2019). Common risk factors for major noncommunicable disease, a systematicoverview of reviews and commentary: the implied potential for targeted riskreduction. Therapeutic Advances in Chronic Disease, 10. https://doi.org/10.1177/2040622319880392
Rasul, F. B., Kalmus, O., Sarker, M., Adib, H. I., Hossain, M. S., Hasan, M. Z., Brenner, S., Nazneen, S., Islam, M. N., & De Allegri, M. (2019). Determinants of health seeking behavior for chronic non-communicable diseases and related out-of-pocket expenditure: results from a cross-sectional survey in northern Bangladesh. Journal of Health, Population and Nutrition, 38(1), 48. https://doi.org/10.1186/s41043-019-0195-z
Segawa, H. K., Uematsu, H., Dorji, N., Wangdi, U., Dorjee, C., Yangchen, P., Kunisawa, S., Sakamoto, R., & Imanaka, Y. (2021). Gender with marital status, cultural differences, and vulnerability to hypertension: Findings from the national survey for noncommunicable disease risk factors and mental health using WHO STEPS in Bhutan. PLOS ONE, 16(8), e0256811. https://doi.org/10.1371/JOURNAL.PONE.0256811
Setyonaluri, D., & Aninditya, F. (2019). Transisi Demografi dan Epidemiologi: Permintaan Pelayanan Kesehatan di Indonesia. In Badan Perencanaan dan Pembangunan Nasional.
Wang, D. D., Li, Y., Bhupathiraju, S. N., Rosner, B. A., Sun, Q., Giovannucci, E. L., Rimm, E. B., Manson, J. A. E., Willett, W. C., Stampfer, M. J., & Hu, F. B. (2021). Fruit and vegetable intake and mortality. Circulation, 143(17), 1642–1654. https://doi.org/10.1161/CIRCULATIONAHA.120.048996
Wekesah, F. M., Nyanjau, L., Kibachio, J., Mutua, M. K., Mohamed, S. F., Grobbee, D. E., Klipstein-Grobusch, K., Ngaruiya, C., Haregu, T. N., Asiki, G., & Kyobutungi, C. K. (2018). Individual and household level factors associated with presence of multiple non-communicable disease risk factors in Kenyan adults. BMC Public Health, 18(Suppl 3). https://doi.org/10.1186/s12889-018-6055-8
World Health Organization. (2018). Global Status Report on Alcohol adn Health 2018. WHO.
World Health Organization. (2021). Noncommunicable diseases. https://www.who.int/news-room/fact-sheets/detail/noncommunicable-diseases
Zatońska, K., Psikus, P., Basiak-Rasała, A., Stępnicka, Z., Gaweł-Dabrowska, D., Wołyniec, M., Gibka, J., Szuba, A., & Połtyn-Zaradna, K. (2021). Obesity and Chosen Non-Communicable Diseases in PURE Poland Cohort Study. International Journal of Environmental Research and Public Health, 18(5), 1–10. https://doi.org/10.3390/IJERPH18052701
Copyright (c) 2023 Ika Puspita Asturiningtyas, Hadi Ashar, Sidiq Purwoko, Nissa Noor Annashr

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
Authors retain copyright and grant the journal right of first publication with the work simultaneously licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License that allows others to share the work with an acknowledgment of the work's authorship and initial publication in this journal.
Authors are able to enter into separate, additional contractual arrangements for the non-exclusive distribution of the journal's published version of the work (e.g., post it to an institutional repository or publish it in a book), with an acknowledgment of its initial publication in this journal.
Authors are permitted to publish their work online in third parties as it can lead to wider dissemination of the work.






