The Influence of Sehat Jiwa Education on the First Active Phase of Labor in Community Health Centers across Makassar City
Abstract
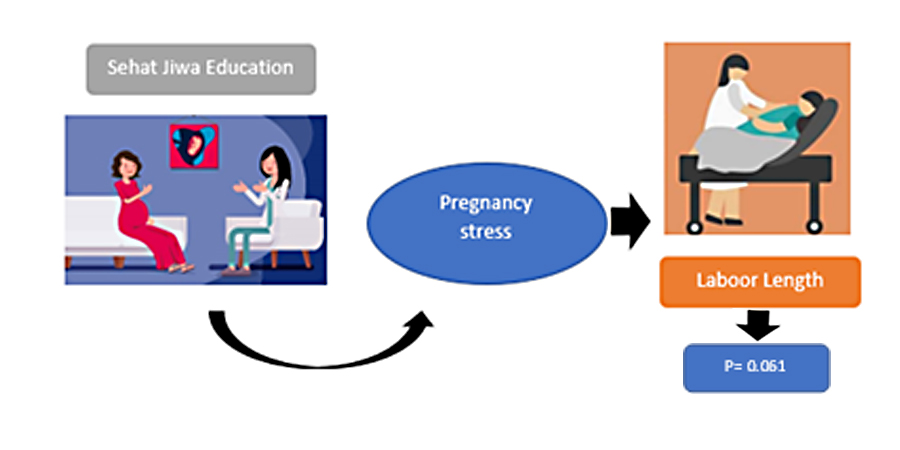
During pregnancy, women commonly experience both psychological and emotional changes, leading to concerns about childbirth and potential labor complications. Therefore, education programs became essential for preparing mothers mentally for delivery with the engagement of health workers and families. This study aimed to assess the effectiveness of Sehat Jiwa education on the length of the first active stage of labor. Using a Quasi-experimental design with a two-group control approach, the sample comprised 64 respondents (34 in the intervention group and 30 in the control group). The instruments adopted were the Sehat Jiwa (English: Soul Health) education module, questionnaires, and partograph sheets. The results showed that there was no significant difference in the length of the first active phase between the intervention and control groups, with a p-value of 0.061 > 0.05. However, the average duration for the intervention group (5.88 hours) was slightly shorter than the control group (6.40 hours). Emphasizing Sehat Jiwa-based education for pregnant women was crucial, fostering smoother delivery processes and reducing the likelihood of increased labor complications.
Downloads
References
Agampodi, T., Katumuluwa, S., Pattiyakumbura, T., Rankaduwa, N., Dissanayaka, T., & Agampodi, S. (2019). Feasibility of incorporating mindfulness based mental health promotion to the pregnancy care program in Sri Lanka: A pilot study. F1000Research, 7, 1–15. https://doi.org/10.12688/f1000research.17049.1
Amiri, P., Mirghafourvand, M., Esmaeilpour, K., Kamalifard, M., & Ivanbagha, R. (2019). The effect of distraction techniques on pain and stress during labor: A randomized controlled clinical trial. BMC Pregnancy and Childbirth, 19(1), 1–9. https://doi.org/10.1186/s12884-019-2683-y
Arlym, L. T., & Herawati, Y. (2021). Edukasi Persiapan Persalinan Pada Pasangan Hamil Dalam Menyambut Persalinan Minim Trauma. Jurnal Kreativitas Pengabdian Kepada Masyarakat (PKM), 4(5), 1117-1123. https://doi.org/10.33024/jkpm.v4i5.4247
Braig, S., Logan, C. A., Reister, F., Rothenbacher, D., & Genuneit, J. (2020). Psychosocial stress and longitudinally measured gestational weight gain throughout pregnancy: The Ulm SPATZ Health Study. Scientific Reports, 10(1), 1–8. https://doi.org/10.1038/s41598-020-58808-8
Dönmez, A., & Karaçam, Z. (2017). The Emotional Favor Mother: Jean Ball Of Deck-Chair Theory. The Journal of Tepecik Education and Research Hospital, 27(1), 7–12. https://doi.org/10.5222/terh.2017.007
Esfandiari, M., Faramarzi, M., Nasiri-Amiri, F., Parsian, H., Chehrazi, M., Pasha, H., Omidvar, S., & Gholinia, H. (2020). Effect of supportive counseling on pregnancy-specific stress, general stress, and prenatal health behaviors: A multicenter randomized controlled trial. Patient Education and Counseling, 103(11), 2297–2304. https://doi.org/10.1016/j.pec.2020.04.024
Firouzbakht, M., Nikpour, M., Khefri, S., Jamali, B., Kazeminavaee, F., & Didehdar, M. (2015). The effectiveness of prenatal intervention on pain and anxiety during the process of Childbirth-Northern Iran: Clinical trial study. Annals of Medical and Health Sciences Research, 5(5), 348. https://doi.org/10.4103/2141-9248.165260
Frety, E. E. (2021). Relationship of Quality of Antenatal Care (ANC) to Stunting Events in Children Age 24-59 Months In Indonesia Using Literature Review Method. MIKIA: Mimbar Ilmiah Kesehatan Ibu dan Anak (Maternal and Neonatal Health Journal), 65-75. https://doi.org/10.36696/mikia.v5i1.61
Hill, N. T. M., Bailey, E., Benson, R., Cully, G., Kirtley, O. J., Purcell, R., Rice, S., Robinson, J., & Walton, C. C. (2022). Researching the researchers: psychological distress and psychosocial stressors according to career stage in mental health researchers. BMC Psychology, 10(1), 1–14. https://doi.org/10.1186/s40359-022-00728-5
Holzman, C., Senagore, P., Tian, Y., Bullen, B., Devos, E., Leece, C., Zanella, A., Fink, G., Rahbar, M. H., & Sapkal, A. (2009). Maternal catecholamine levels in midpregnancy and risk of preterm delivery. American Journal of Epidemiology, 170(8), 1014–1024. https://doi.org/10.1093/aje/kwp218
Innab, A., Al-khunaizi, A., Al-otaibi, A., & Moafa, H. (2023). Effects of mindfulness-based childbirth education on prenatal anxiety: A quasi-experimental study. Acta Psychologica, 238(July), 103978. https://doi.org/10.1016/j.actpsy.2023.103978
Jesica, F., & Friadi, A. (2019). Hubungan Kadar Kortisol Dan Prostaglandin Maternal Dengan Persalinan Preterm Dan Aterm. Jurnal Ilmu Keperawatan Dan Kebidanan, 10(1), 21. https://doi.org/10.26751/jikk.v10i1.540
Kuo, T. C., Au, H. K., Chen, S. R., Chipojola, R., Lee, G. T., Lee, P. H., & Kuo, S. Y. (2022). Effects of an integrated childbirth education program to reduce fear of childbirth, anxiety, and depression, and improve dispositional mindfulness: A single-blind randomised controlled trial. Midwifery, 113, 103438. https://doi.org/10.1016/j.midw.2022.103438
Koushede, V., Brixval, C. S., Axelsen, S. F., Lindschou, J., Winkel, P., Maimburg, R. D., & Due, P. (2013). Group-based antenatal birth and parent preparation for improving birth outcomes and parenting resources: Study protocol for a randomised trial. Sexual & Reproductive Healthcare, 4(3), 121–126. https://doi.org/https://doi.org/10.1016/j.srhc.2013.08.003
Koushede, V., Brixval, C. S., Thygesen, L. C., Axelsen, S. F., Winkel, P., Lindschou, J., Gluud, C., & Due, P. (2017). Antenatal small-class education versus auditorium-based lectures to promote positive transitioning to parenthood - A randomised trial. PLoS ONE, 12(5), 1–17. https://doi.org/10.1371/journal.pone.0176819
Kowalska, J. (2023). The Level of Stress and Anxiety in Pregnant Women Depending on Social Support and Physical Activity. Journal of Clinical Medicine, 12(9). https://doi.org/10.3390/jcm12093143
Lönnberg, G., Jonas, W., Unternaehrer, E., Bränström, R., Nissen, E., & Niemi, M. (2020). Effects of a mindfulness based childbirth and parenting program on pregnant women’s perceived stress and risk of perinatal depression–Results from a randomized controlled trial. Journal of Affective Disorders, 262(October 2019), 133–142. https://doi.org/10.1016/j.jad.2019.10.048
Marwang, S., Masni, M., Stang, S., Mallongi, A., Sudirman, J., & Triananinsi, N. (2020). The impact of his frequency and religiosity toward prolonged second stage and its impact of the placenta separation in maternity at siti fatimah hospital Makassar. Open Access Macedonian Journal of Medical Sciences, 8(T2), 200–203. https://doi.org/10.3889/oamjms.2020.5228
Marwang, S., Passe, R., Aswan, R., Triananinsi, N., Iskandar, N., Ohorella, F., & Sikki, S. (2020). Effects of classical music therapy on anxiety level of caesarean section mother. Medico-Legal Update, 20(3), 806–810. https://doi.org/10.37506/mlu.v20i3.1500
Miller, P. G. T., Sinclair, M., Gillen, P., McCullough, J. E. M., Miller, P. W., Farrell, D. P., Slater, P. F., Shapiro, E., & Klaus, P. (2021). Early psychological interventions for prevention and treatment of post-traumatic stress disorder (PTSD) and post-traumatic stress symptoms in post-partum women: A systematic review and meta-analysis. PLoS ONE, 16(11 November), 1–25. https://doi.org/10.1371/journal.pone.0258170
Moulana, F., Martadiansyah, A., & Liberty, I. A. (2019). Risk Factors of Postpartum Hemorrhage in Rsup Dr. Mohammad Hoesin. Majalah Kedokteran Sriwijaya, 51(2), 63–72. https://doi.org/10.32539/mks.v51i2.8534
Mueller, N. T., Zhang, M., Juraschek, S. P., Miller, E. R., & Appel, L. J. (2020). Effects of high-fiber diets enriched with carbohydrate, protein, or unsaturated fat on circulating short chain fatty acids: results from the OmniHeart randomized trial. The American Journal of Clinical Nutrition, 111(3), 545–554. https://doi.org/10.1093/ajcn/nqz322
Ngai, F. W., & Xiao, X. (2021). Perceptions of paternal involvement and labour pain management in Chinese couples during childbirth: A qualitative study. Women and Birth, 34(3), 288–295. https://doi.org/10.1016/j.wombi.2020.03.003
Noviyanti, A., & Jasmi, J. (2022). Faktor Fisik dan Psikologis Ibu Bersalin dengan Intensitas Nyeri Persalinan Kala I pada Ibu Primipara. Jurnal Kesehatan, 13(3), 437. https://doi.org/10.26630/jk.v13i3.2945
Nowacka, U., Kozlowski, S., Januszewski, M., Sierdzinski, J., Jakimiuk, A., & Issat, T. (2021). Covid-19 pandemic-related anxiety in pregnant women. International Journal of Environmental Research and Public Health, 18(14). https://doi.org/10.3390/ijerph18147221
Pan, W. L., Chang, C. W., Chen, S. M., & Gau, M. L. (2019). Assessing the effectiveness of mindfulness-based programs on mental health during pregnancy and early motherhood - A randomized control trial. BMC Pregnancy and Childbirth, 19(1), 1–8. https://doi.org/10.1186/s12884-019-2503-4
Papapetrou, C., Panoulis, K., Mourouzis, I., & Kouzoupis, A. (2020). Pregnancy and the perinatal period: The impact of attachment theory. Psychiatrike = Psychiatriki, 31(3), 257–270. https://doi.org/10.22365/jpsych.2020.313.257
Răchită, A. I. C., Strete, G. E., Suciu, L. M., Ghiga, D. V., Sălcudean, A., & Mărginean, C. (2022). Psychological Stress Perceived by Pregnant Women in the Last Trimester of Pregnancy. International Journal of Environmental Research and Public Health, 19(14), 1–10. https://doi.org/10.3390/ijerph19148315
Rejeki, S., Hartiti, T., & Khayati, N. (2014). Nyeri Persalinan Kala I Melalui Praktik Counter-Pressure Oleh Suami Di RSUD Soewondo Kendal. Jurnal Keperawatan Maternitas, 2(2), 127–135.
Rempel, L. M., Körber, H., Reichler, I. M., Balogh, O., & Goericke-Pesch, S. (2021). Investigations on the potential role of prostaglandin E2 in canine uterine inertia. Theriogenology, 175, 134–147. https://doi.org/10.1016/j.theriogenology.2021.09.003
Saharoy, R., Potdukhe, A., Wanjari, M., & Taksande, A. B. (2023). Postpartum Depression and Maternal Care: Exploring the Complex Effects on Mothers and Infants. Cureus, 15(7). https://doi.org/10.7759/cureus.41381
Sari, E., & Handayani, W. (2023). Hubungan Tingkat Stres Dengan Lama Fase Aktif Kala 1 Persalinan Pada Primigravida di BPM Rita. Journal on Education, 06(01), 2939–2949. https://doi.org/10.31004/joe.v6i1.3337
Schaper, C. (2020). Competitive Inhibition of Cortisol by Prostaglandins at the Ligand Binding Domain of Glucocorticoid Receptors. BioRxiv, 1–22. https://www.biorxiv.org/content/10.1101/851501v7.abstract
Sharma, N., Vyas, H., & Singh, P. (2022). Effectiveness of Childbirth Education Programme on Knowledge , Intrapartum Behavior , and Pregnancy Outcome Among Selected Primigravida Mothers At Aiims. European Journal of Molecular & Clinical Medicine, 9(4), 1680–1690.
Smith, C. A., Levett, K. M., Collins, C. T., Armour, M., Dahlen, H. G., & Suganuma, M. (2018). Relaxation techniques for pain management in labour. Cochrane Database of Systematic Reviews, 2018(3). https://doi.org/10.1002/14651858.CD009514.pub2
Stang, S., Selin, D., Suriah, S., Marwang, S., Mallongi, A., & Ishak, H. (2020). The effect of educational media development in increasing knowledge and attitudes on pregnancy complications at sayang rakyat hospital in makassar. Open Access Macedonian Journal of Medical Sciences, 8(T2), 196–199. https://doi.org/10.3889/oamjms.2020.5227
Sudirman, J., Bachri, N., Syafar, M., Jusuf, E. C., Syamsuddin, S., Mappaware, N. A., & Saleng, H. (2022). Foot Hydrotherapy: Non-pharmacology Treatment for Reducing Anxiety in Third Trimester Pregnancy. Open Access Macedonian Journal of Medical Sciences, 10, 320–323. https://doi.org/10.3889/oamjms.2022.8271
Syamsuddin, S., Ahmad, M., & Mappaware, N. A. (2022). Correlation Prenatal Distress Questionnaires Score And Cortisol Serum Levels For Pregnant Women. 04, 9–14. https://doi.org/10.17605/OSF.IO/BYJ8D
Szóstek-Mioduchowska, A. Z., Shiotani, H., Yamamoto, Y., Sadowska, A., Wójtowicz, A., Kozai, K., Hojo, T., Kimura, K., Skarzynski, D. J., & Okuda, K. (2021). Effects of cortisol on prostaglandin F2α secretion and expression of genes involved in the arachidonic acid metabolic pathway in equine endometrium - In vitro study: Cortisol regulation of endometrial prostaglandin F2α in mare. Theriogenology, 173, 221–229. https://doi.org/10.1016/j.theriogenology.2021.08.009
Tachibana, Y., Koizumi, N., Akanuma, C., Tarui, H., Ishii, E., Hoshina, T., Suzuki, A., Asano, A., Sekino, S., & Ito, H. (2019). Integrated mental health care in a multidisciplinary maternal and child health service in the community: the findings from the Suzaka trial. BMC Pregnancy and Childbirth, 19. https://doi.org/http://dx.doi.org/10.1186/s12884-019-2179-9
Walter, M. H., Abele, H., & Plappert, C. F. (2021). The Role of Oxytocin and the Effect of Stress During Childbirth: Neurobiological Basics and Implications for Mother and Child. Frontiers in Endocrinology, 12(October), 1–10. https://doi.org/10.3389/fendo.2021.742236
Ying, L., Wu, L. H., & Loke, A. Y. (2016). The effects of psychosocial interventions on the mental health, pregnancy rates, and marital function of infertile couples undergoing in vitro fertilization: a systematic review. Journal of Assisted Reproduction and Genetics, 33(6), 689–701. https://doi.org/10.1007/s10815-016-0690-8
Copyright (c) 2023 Sumarni Marwang, Rosita Passe, Nurhidayat Triananingsih, Rahayu Eriyanti Kusniyanto

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
Authors retain copyright and grant the journal right of first publication with the work simultaneously licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License that allows others to share the work with an acknowledgment of the work's authorship and initial publication in this journal.
Authors are able to enter into separate, additional contractual arrangements for the non-exclusive distribution of the journal's published version of the work (e.g., post it to an institutional repository or publish it in a book), with an acknowledgment of its initial publication in this journal.
Authors are permitted to publish their work online in third parties as it can lead to wider dissemination of the work.






