Environmental Sanitation as Risk Factors for Intestinal Protozoa Infection among Stunted Children in Sugerkidul Village, Indonesia
Abstract
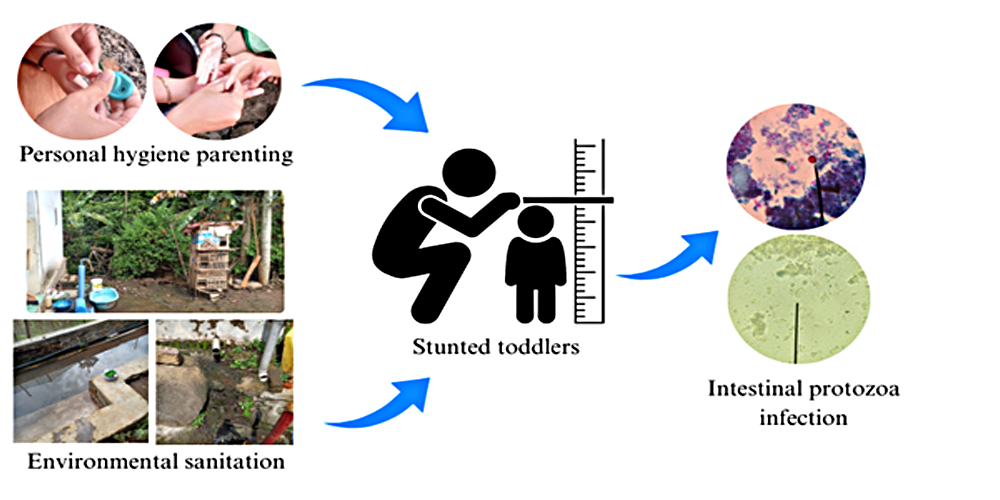
Stunting, a prevalent health issue in Indonesia, has been found to have a significant impact on the overall well-being of children, with a prevalence rate of 24.4%. This condition not only affects physical growth but also puts children at a heightened risk of various infections, including those caused by intestinal protozoa. Therefore, this study aimed to determine the relationship between personal hygiene parenting style and environmental sanitation with intestinal protozoa infection among stunted children in Sugerkidul Village, Jember District, Indonesia. The participants included were 30 stunted children. Questionnaires were used to collect data on personal hygiene parenting style and environmental sanitation, while microscopic stool examination was conducted to identify intestinal protozoa infection. The results showed that 26.7% of stunted children were infected with intestinal protozoa such as Giardia lamblia (13.3%), Blastocystis hominins (3.3%), and Cryptosporidium parvum (10%). Statistical analysis using Fisher's exact test showed a significant association between environmental sanitation and intestinal protozoa infection. However, there was no association between personal hygiene parenting style and this infection among stunted children in Sugerkidul Village. Therefore, to prevent intestinal protozoa infection, it is necessary to improve environmental sanitation.
Downloads
References
Infection and undernutrition increase the risk of stunting among rural children. International Journal of Public Health Science, 11(3), 920–926. https://doi.org/10.11591/ijphs.v11i3.21592
Bahmani, P., Maleki, A., Sadeghi, S., Shahmoradi, B., & Ghahremani, E. (2017). Prevalence of intestinal protozoa infections and associated risk factors among schoolchildren in Sanandaj City, Iran. Iranian Journal of Parasitology, 12(1), 108–116. https://pubmed.ncbi.nlm.nih.gov/28761467/
Balbino, L. F., Filho, A. A., Farias, B. E. S., Costa, G. V., Sinhorin, G. H., Silva, L. L. S., Marques, R. C. R., Jucá, F. L., Brilhante, A. F., & Melchior, L. A. K. (2023). Intestinal protozoan infections and environment conditions among rural schoolchildren in Western Brazilian Amazon. Brazilian Journal of Biology, 83, 1–4. https://doi.org/10.1590/1519-6984.247530
Bednarska, M., Jankowska, I., Pawelas, A., Piwczyńska, K., Bajer, A., Wolska-Kuśnierz, B., Wielopolska, M., & Welc-Falęciak, R. (2018). Prevalence of Cryptosporidium, Blastocystis, and other opportunistic infections in patients with primary and acquired immunodeficiency. Parasitology Research, 117(9), 2869–2879. https://doi.org/10.1007/s00436-018-5976-6
Berhe, B., Mardu, F., Tesfay, K., Legese, H., Adhanom, G., Haileslasie, H., Gebremichail, G., Tesfanchal, B., Shishay, N., & Negash, H. (2020). More than half prevalence of protozoan parasitic infections among diarrheic outpatients in eastern tigrai, ethiopia, 2019; a cross-sectional study. Infection and Drug Resistance, 13, 27–34. https://doi.org/10.2147/IDR.S238493
Boughattas, S., Behnke, J. M., Al-Ansari, K., Sharma, A., Abu-Alainin, W., Al-Thani, A., & Abu-Madi, M. A. (2017). Molecular analysis of the enteric protozoa associated with acute diarrhea in hospitalized children. Frontiers in Cellular and Infection Microbiology, 7(343), 1–10. https://doi.org/10.3389/fcimb.2017.00343
Deka, S., Kalita, D., & Hazarika, N. K. (2022). Prevalence and Risk Factors of Intestinal Parasitic Infection in Under‑Five Children With Malnutrition: A Hospital Based Cross‑Sectional Study. Journal of Family Medicine and Primary Care, 11(6), 2794–2801. https://doi.org/10.4103/jfmpc.jfmpc_1742_21
Dobo, B. (2018). Prevalence of intestinal protozoan infection among patients in Hawassa city administration millennium health center, Ethiopia. Journal of Applied Biotechnology & Bioengineering, 5(4), 206–210. https://doi.org/10.15406/jabb.2018.05.00139
El-Aal, B. G. A., Nady, S. E., Shokr, E. A., & Shokry, M. W. (2022). Awareness And Practices Of Preventive Behaviors Toward Intestinal Parasitic Infection Among Mothers Of Preschool Children. Journal of Positive School Psychology, 6(8), 6290–6305. https://journalppw.com/index.php/jpsp/article/view/10926
Eyasu, A., Molla, M., Kefale, B., Sisay, W., Andargie, Y., Kebede, F., & Jemere, T. (2022). Prevalence and Associated Risk Factors of Endoparasites among Under-Five Children in Debre Tabor Comprehensive Specialized Hospital, Debre Tabor, Northwest Ethiopia: A Cross-Sectional Study. Journal of Parasitology Research, 2022, 1–10. https://doi.org/10.1155/2022/6917355
Fauziah, N., Aviani, J. K., Agrianfanny, Y. N., & Fatimah, S. N. (2022). Intestinal Parasitic Infection and Nutritional Status in Children under Five Years Old: A Systematic Review. Tropical Medicine and Infectious Disease, 7(11), 371. https://doi.org/10.3390/tropicalmed7110371
Fuhrimann, S., Winkler, M. S., Pham-Duc, P., Do-Trung, D., Schindler, C., Utzinger, J., & Cissé, G. (2016). Intestinal parasite infections and associated risk factors in communities exposed to wastewater in urban and peri-urban transition zones in Hanoi, Vietnam. Parasites and Vectors, 9(1), 1–14. https://doi.org/10.1186/s13071-016-1809-6
Galgamuwa, L., Iddawela, D., & Dharmaratne, S. (2016). Intestinal protozoa infections, associated risk factors and clinical features among children in a low-income tea plantation community in Sri Lanka. International Journal of Community Medicine and Public Health, 3(9), 2452–2458. https://doi.org/10.18203/2394-6040.ijcmph20163053
Gizaw, Z., Adane, T., Azanaw, J., Addisu, A., & Haile, D. (2018). Childhood intestinal parasitic infection and sanitation predictors in rural Dembiya, northwest Ethiopia. Environmental Health and Preventive Medicine, 23(1), 1–10. https://doi.org/10.1186/s12199-018-0714-3
Gizaw, Z., Yalew, A. W., Bitew, B. D., Lee, J., & Bisesi, M. (2022). Stunting among children aged 24–59 months and associations with sanitation, enteric infections, and environmental enteric dysfunction in rural northwest Ethiopia. Scientific Reports, 12(1), 1–11. https://doi.org/10.1038/s41598-022-23981-5
Hajare, S. T., Chekol, Y., & Chauhan, N. M. (2022). Assessment of prevalence of Giardia lamblia infection and its associated factors among government elementary school children from Sidama zone, SNNPR, Ethiopia. PLoS ONE, 17(3), 1–17. https://doi.org/10.1371/journal.pone.0264812
Hajissa, K., Islam, M. A., Sanyang, A. M., & Mohamed, Z. (2022). Prevalence of intestinal protozoan parasites among school children in africa: A systematic review and meta-analysis. PLoS Neglected Tropical Diseases, 16(2), 1–20. https://doi.org/10.1371/journal.pntd.0009971
Hoseinzadeh, E., Rostamian, A., Razaghi, M., & Wei, C. (2021). Waterborne transmission of protozoan parasites: A review of water resources in Iran – An update 2020. Desalination and Water Treatment, 213, 91–105. https://doi.org/10.5004/dwt.2021.26678
Kemenkes RI. (2021). Laporan Kinerja Kementerian Kesehatan 2021. Kementerian Kesehatan Republik Indonesia. http://ppid.kemkes.go.id/uploads/img_62f0d4c9e9f34.pdf
Luz, J. G. G., de Carvalho, A. G., Marques, A. P., Marcondes, A. A., Roma, J. H. F., Castro, L. S., Castro, L. S., Dias, J. V. L., & Pavoni, J. H. C. (2017). Intestinal parasitic infections and associated risk factors in preschoolers from different urban settings in Central-Western Brazil. Asian Pacific Journal of Tropical Disease, 7(7), 405–410. https://doi.org/10.12980/apjtd.7.2017D7-90
Manggala, A. K., Wiswa, K., Kenwa, M., Me, M., Kenwa, L., Agung, A., Dwinaldo, G., Jaya, P., Agung, A., & Sawitri, S. (2018). Risk factors of stunting in children aged 24-59 months Arya. Paediatrica Indonesiana, 58(5), 205–212. http://dx.doi.org/10.14238/pi58.5.2018.205-12
Mengesha, A., Hailu, S., Birhane, M., & Belay, M. M. (2021). The Prevalence of Stunting and Associated Factors among Children Under Five years of age in Southern Ethiopia : Community Based Cross-Sectional Study. 87(1), 1–14. https://doi.org/10.5334/aogh.3432
Mohammed, J., Shiferaw, A., Zeleke, A., Eshetu, Y., Gebeyehu, Z., Ayehu, A., & Adem, Y. (2022). Prevalence and Associated Risk Factors of Intestinal Parasites among Diarrheic Under-Five Children Attending Bahir Dar and Han Health Centers, Northwest Ethiopia: A Cross-Sectional Study. Journal of Parasitology Research, 2022(1), 1–9. https://doi.org/10.1155/2022/7066529
Muhajir, N. F., Herdiana, E., & Mulyaningsih, B. (2019). Study of intestinal protozoa infectio in the hospitalized patients diagnosed with diarrhoea in the Panembahan Senopati hospital. Jurnal Kedokteran Dan Kesehatan Indonesia, 10(2), 176–184. https://doi.org/10.20885/jkki.vol10.iss2.art10
Muryanti, Dharmawan, R., & Murti, B. (2016). The Relationship Between Maternal Education, Family Income, Parenting Style, and Language Development in Children Aged 3-4 Years in Boyolali, Central Java. Indonesian Journal of Medicine, 1(2), 100–107. https://doi.org/10.26911/theijmed.2016.01.02.03
Njambi, E., Magu, D., Masaku, J., Okoyo, C., & Njenga, S. M. (2020). Prevalence of Intestinal Parasitic Infections and Associated Water, Sanitation, and Hygiene Risk Factors among School Children in Mwea Irrigation Scheme, Kirinyaga County, Kenya. Journal of Tropical Medicine, 2020(1), 1–9. https://doi.org/10.1155/2020/3974156
Ntulume, I., Tibyangye, J., Aliero, A., & Banson, B. (2017). Prevalence of Intestinal Protozoan Infections and the Associated Risk Factors among Children in Bushenyi District, Western Uganda. International Journal of Tropical Disease & Health, 23(2), 1–9. https://doi.org/10.9734/ijtdh/2017/33255
Pérez Pico, A. M., Álvarez, E. M., Rodríguez, J. V., & Acevedo, R. M. (2022). Differences in Hygiene Habits among Children Aged 8 to 11 Years by Type of Schooling. Children, 9(2), 1–16. https://doi.org/10.3390/children9020129
Rajoo, Y., Ambu, S., Lim, Y. A. L., Rajoo, K., Tey, S. C., Lu, C. W., & Ngui, R. (2017). Neglected intestinal parasites, malnutrition and associated key factors: A population based cross-sectional study among indigenous communities in sarawak, Malaysia. PLoS ONE, 12(1), 1–17. https://doi.org/10.1371/journal.pone.0170174
Salehi Kahish, R., Alghasi, A., Hadadi, S., Nasab, M. A., & Mafakherzadeh, A. (2021). The prevalence of blastocystis infection in pediatric patients with malignancy: A single-center study in Ahvaz, Iran. Archives of Pediatric Infectious Diseases, 9(2), 1–5. https://doi.org/10.5812/pedinfect.104068
Siddiqa, M., Zubair, A., Kamal, A., Ijaz, M., & Abushal, T. (2022). Prevalence and associated factors of stunting , wasting and underweight of children below five using quintile regression analysis ( PDHS 2017 – 2018 ). Scientific Reports, 1–8. https://doi.org/10.1038/s41598-022-24063-2
Taddese, A. A., Dagnew, B., Dagne, H., & Andualem, Z. (2020). Mother’s Handwashing Practices and Health Outcomes of Under-Five Children in Northwest Ethiopia. Pediatric Health, Medicine and Therapeutics, 11(1), 101–108. https://doi.org/10.2147/phmt.s238392
Tambunan, Y. R., & Panggabean, Y. C. (2021). The Correlation between Personal Hygiene and Intestinal Parasitic Infection in Students of SDN 060889, SDN 060894, and SDN 060831 Medan. Journal of Endocrinology, Tropical Medicine, and Infectious Disease (JETROMI), 3(3), 78–84. https://doi.org/10.32734/jetromi.v3i3.3550
Tamomh, A. G., Agena, A. E. M., Elamin, E., Suliman, M. A., Elmadani, M., Omara, A. B., & Musa, S. A. (2021). Prevalence of cryptosporidiosis among children with diarrhoea under five years admitted to Kosti teaching hospital, Kosti City, Sudan. BMC Infectious Diseases, 21(1), 1–6. https://doi.org/10.1186/s12879-021-06047-1
Tegen, D., Damtie, D., & Hailegebriel, T. (2020). Prevalence and Associated Risk Factors of Human Intestinal Protozoan Parasitic Infections in Ethiopia: A Systematic Review and Meta-Analysis. Journal of Parasitology Research, 2020(1), 1–15. https://doi.org/10.1155/2020/8884064
Titaley, C. R., Ariawan, I., Hapsari, D., Muasyaroh, A., & Dibley, M. J. (2019). Determinants of the stunting of children under two years old in Indonesia: A multilevel analysis of the 2013 Indonesia basic health survey. Nutrients, 11(5), 1–13. https://doi.org/10.3390/nu11051106
Tsegaye, B., Yoseph, A., & Beyene, H. (2020). Prevalence and factors associated with intestinal parasites among children of age 6 to 59 months in, Boricha district, South Ethiopia, in 2018. BMC Pediatrics, 20(1), 28. https://doi.org/10.1186/s12887-020-1935-3
Varghese, J. S., Gupta, A., Mehta, R., Stein, A. D., & Patel, S. A. (2022). Changes in Child Undernutrition and Overweight in India From 2006 to 2021: An Ecological Analysis of 36 States. Global Health: Science and Practice, 10(5), 1–10. https://doi.org/10.9745/GHSP-D-21-00569
Wahdini, S., Putra, V. P., & Sungkar, S. (2021). The prevalence of intestinal protozoan infections among children in southwest sumba based on the type of water sources. Infection and Chemotherapy, 53(3), 519–527. https://doi.org/10.3947/ic.2021.0067
Waldram, A., Vivancos, R., Hartley, C., & Lamden, K. (2017). Prevalence of Giardia infection in households of Giardia cases and risk factors for household transmission. BMC Infectious Diseases, 17(1), 1–7. https://doi.org/10.1186/s12879-017-2586-3
Wale, M., & Gedefaw, S. (2022). Prevalence of Intestinal Protozoa and Soil Transmitted Helminths Infections among School Children in Jaragedo Town, South Gondar Zone of Ethiopia. Journal of Tropical Medicine, 2022(1), 1–11. https://doi.org/10.1155/2022/5747978
Wolde, M., Abate, M., Mandefro, G., Beru, E., Kassahun, A., & Tesema, G. A. (2022). Determinants of handwashing practice and its associated factors among mothers of under-5 children in Kolladiba town, Northwest Ethiopia: Cross-sectional study. BMJ Open, 12(6). https://doi.org/10.1136/bmjopen-2021-058960
Yoseph, A., & Beyene, H. (2020). The high prevalence of intestinal parasitic infections is associated with stunting among children aged 6-59 months in Boricha Woreda, Southern Ethiopia: A cross-sectional study. BMC Public Health, 20(1), 1–13. https://doi.org/10.1186/s12889-020-09377-y
Zemene, T., & Shiferaw, M. B. (2018). Prevalence of intestinal parasitic infections in children under the age of 5 years attending the Debre Birhan referral hospital, North Shoa, Ethiopia. BMC Research Notes, 11(1), 1–6. https://doi.org/10.1186/s13104-018-3166-3.
Copyright (c) 2023 Hanu Neda Septian, Erma Sulistyaningsih, Angga Mardro Raharjo, Bagus Hermansyah, Wiwien Sugih Utami, Yunita Armiyanti

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
Authors retain copyright and grant the journal right of first publication with the work simultaneously licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License that allows others to share the work with an acknowledgment of the work's authorship and initial publication in this journal.
Authors are able to enter into separate, additional contractual arrangements for the non-exclusive distribution of the journal's published version of the work (e.g., post it to an institutional repository or publish it in a book), with an acknowledgment of its initial publication in this journal.
Authors are permitted to publish their work online in third parties as it can lead to wider dissemination of the work.






