Complete Basic Immunization of Children 12-23 Months Based on Geographical Differences and Determinants of Utilization
Abstract
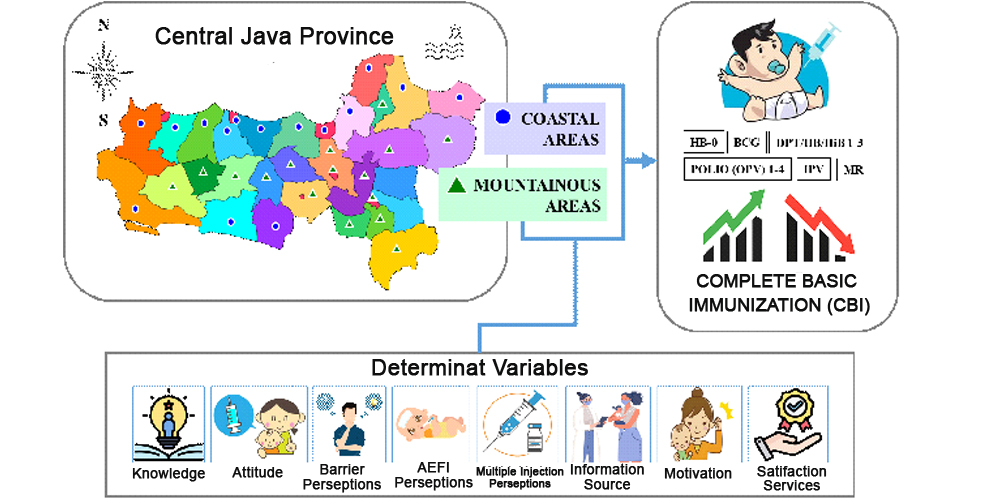
Although immunization has been proven to be cost-effective in preventing dangerous infectious diseases, its complete utilization is not optimal. Therefore, this study aims to analyze the Complete Basic Immunization (CBI) coverage among children aged 12-23 months based on differences in geographical characteristics areas, and factors influencing its utilization. This was an analytic study conducted with a quantitative method and cross-sectional approach, and was carried out in 31 districts in Central Java Province, which were categorized into coastal and mountainous areas. The target population included all children aged 12-23 months, and a sample of 685 children was selected using a purposive sampling technique. The collected data were analyzed using independent t-test for numerical, and chi-square for categorical data. Based on the results, the CBI coverage did not differ between children living in coastal and mountainous areas, except for HB-0, BCG, and DPT/HB/HiB-1 immunizations which were significantly different. Furthermore, the mean score of attitudes, perceptions (about barriers, AEFI, multiple injections), information sources, motivation, and service satisfaction among children living in coastal areas were higher and proved to be significantly different from those living in mountainous areas. Access to healthcare facilities and their availability also emerged as a differentiating factor between the two areas. To improve CBI utilization, effective strategies include using appropriate communication, information, and socialization media, particularly through internet technology. These strategies should be integrated into Information, Education, and Communication (IEC) program, alongside improving access and immunization service systems.
Downloads
References
Ahmad, N., & Syuhada, A. D. (2020). Penerimaan Orang Tua Terhadap Vaksin Polio Suntik (IVP) di Kota Cimahi. PIN-LITAMAS, 2(1), 28-31. http://ejournal.stikesjayc.id/index.php/PLT/article/view/6
Al-lela, Q. B. O., Bahari, M. B., Al-Qazaz, H. K., Salih, M. R., Jamshed, S. Q., & Elkalmi, R. M. (2014). Are parents' knowledge and practice regarding immunization related to pediatrics’ immunization compliance? a mixed method study. BMC pediatrics, 14, 1-7. https://doi.org/10.1186/1471-2431-14-20
Allan, S., Adetifa, I. M., & Abbas, K. (2021). Inequities in childhood immunisation coverage associated with socioeconomic, geographic, maternal, child, and place of birth characteristics in Kenya. BMC infectious diseases, 21(1), 553. https://doi.org/10.1186/s12879-021-06271-9
Amalia, A. N., Iriani, Y., & Lestari, H. I. (2017). Faktor-Faktor yang Mempengaruhi Terjadinya Missed Opportunities Vaksinasi Program Pengembangan Imunisasi (PPI) pada Anak Berusia Kurang dari Tiga Tahun di Kecamatan Sukarame Palembang. Majalah Kedokteran Sriwijaya, 49(1), 10-17. https://doi.org/10.36706/mks.v49i1.8319
An, D. T. M., Lee, J. K., Minh, H. V., Trang, N. T. H., Huong, N. T. T., Nam, Y. S., & Dung, D. V. (2016). Timely immunization completion among children in Vietnam from 2000 to 2011: a multilevel analysis of individual and contextual factors. Global health action, 9(1), 29189. https://doi.org/10.3402/gha.v9.29189
Arnault, D. S., & Woo, S. (2018). Testing the influence of cultural determinants on help-seeking theory. American Journal of Orthopsychiatry, 88(6), 650. https://psycnet.apa.org/doi/10.1037/ort0000353
Barrera, L., Trumbo, S. P., Bravo-Alcántara, P., Velandia-González, M., & Danovaro-Holliday, M. (2014). From the parents’ perspective: a user-satisfaction survey of immunization services in Guatemala. BMC public health, 14(1), 1-11. https://doi.org/10.1186/1471-2458-14-231
Browne, M., Thomson, P., Rockloff, M. J., & Pennycook, G. (2015). Going against the herd: psychological and cultural factors underlying the ‘vaccination confidence gap’. PLoS one, 10(9), e0132562. https://doi.org/10.1371/journal.pone.0132562
Carolina, A. R., Efendi, D., & Kurniasari, M. D. (2021). Determinant factor of childhood basic immunization compliance during the COVID-19 pandemic in Jambi City, Jambi Province, Indonesia. Journal of Nursing Practice, 5(1), 77-88. https://doi.org/10.30994/jnp.v5i1.154
Chan, M. (2014). The contribution of immunization: saving millions of lives, and more. Public Health Reports, 129(5_suppl3), 7-8. https://doi.org/10.1177%2F00333549141295S303
Crocker-Buque, T., Mindra, G., Duncan, R., & Mounier-Jack, S. (2017). Immunization, urbanization and slums–a systematic review of factors and interventions. BMC public health, 17, 1-16. https://doi.org/10.1186/s12889-017-4473-7
Debela, B. G., Negassa, B., Hareru, H. E., Sisay, D., & Soboksa, N. E. (2022). Maternal satisfaction on child immunization services of rural health extension workers in Dawie Harewa district, Northeast Ethiopia: A community based cross-sectional study. Environmental Challenges, 7, 100455. https://doi.org/10.1016/j.envc.2022.100455
Defar, A., Okwaraji, Y. B., Tigabu, Z., Persson, L. Å., & Alemu, K. (2019). Geographic differences in maternal and child health care utilization in four Ethiopian regions; a cross-sectional study. International journal for equity in health, 18(1), 1-11. https://doi.org/10.1186/s12939-019-1079-y
Ebile Akoh, W., Ateudjieu, J., Nouetchognou, J. S., Yakum, M. N., Djouma Nembot, F., Nafack Sonkeng, S., Sonkeng, S. N., Fopa, M. S., & Watcho, P. (2016). The expanded program on immunization service delivery in the Dschang health district, west region of Cameroon: a cross sectional survey. BMC public health, 16, 1-8. https://doi.org/10.1186/s12889-016-3429-7
Eden, L. M., Macintosh, J. L., Luthy, K. E., & Beckstrand, R. L. (2014). Minimizing pain during childhood vaccination injections: improving adherence to vaccination schedules. https://doi.org/10.2147/PHMT.S50510
Efendi, F., Pradiptasiwi, D. R., Krisnana, I., Kusumaningrum, T., Kurniati, A., Sampurna, M. T. A., & Berliana, S. M. (2020). Factors associated with complete immunizations coverage among Indonesian children aged 12–23 months. Children and Youth Services Review, 108, 104651. https://doi.org/10.1016/j.childyouth.2019.104651
Elran, B., Yaari, S., Glazer, Y., Honovich, M., Grotto, I., & Anis, E. (2018). Parents' perceptions of childhood immunization in Israel: Information and concerns. Vaccine, 36(52), 8062-8068. https://doi.org/10.1016/j.vaccine.2018.10.078
Fefferman, N. H., & Naumova, E. N. (2015). Dangers of vaccine refusal near the herd immunity threshold: a modelling study. The Lancet Infectious Diseases, 15(8), 922-926. https://doi.org/10.1016/S1473-3099(15)00053-5
Galadima, A. N., Zulkefli, N. A. M., Said, S. M., & Ahmad, N. (2021). Factors influencing childhood immunisation uptake in Africa: a systematic review. BMC Public Health, 21(1), 1-20. https://doi.org/10.1186/s12889-021-11466-5
Handayani, N. M. S., & Kardiwinata, M. P. (2021). Pemetaan cakupan imunisasi MR dan kasus campak rubella di Provinsi Bali tahun 2019. Archive of Community Health, 8(1), 109-123. https://doi.org/10.24843/ACH.2021.v08.i01.p08
Hardhantyo, M., & Chuang, Y. C. (2021). Urban-rural differences in factors associated with incomplete basic immunization among children in Indonesia: a nationwide multilevel study. Pediatrics & Neonatology, 62(1), 80-89. https://doi.org/10.1016/j.pedneo.2020.09.004
Harizon, I., Misnaniarti, M., & Idris, H. (2020). Faktor Pemanfaatan Imunisasi Inactivated Polio Vaccine (IPV). Jurnal Kesehatan, 11(1), 19-28. http://dx.doi.org/10.26630/jk.v11i1.1136
Harmasdiyani, R. (2015). The Influence of Mother’s Characteristics Toward Basic Complete Immunization Non-Compliance for Children Under-Two-Years. Jurnal Berkala Epidemiologi, 3 (3), 304–314. https://doi.org/10.20473/jbe.V3I32015.304-314
Herliana, P., & Douiri, A. (2017). Determinants of immunisation coverage of children aged 12–59 months in Indonesia: a cross-sectional study. BMJ open, 7(12), e015790. http://dx.doi.org/10.1136/bmjopen-2016-015790
Hu, Y., Chen, Y., Guo, J., Tang, X., & Shen, L. (2014). Completeness and timeliness of vaccination and determinants for low and late uptake among young children in eastern China. Human vaccines & immunotherapeutics, 10(5), 1408-1415. https://doi.org/10.4161/hv.28054
Joseph, N. K., Macharia, P. M., Ouma, P. O., Mumo, J., Jalang’o, R., Wagacha, P. W., ... & Okiro, E. A. (2020). Spatial access inequities and childhood immunisation uptake in Kenya. BMC public health, 20(1), 1-12. https://doi.org/10.1186/s12889-020-09486-8
Kanchan I., Firoz F., Kurlikar, P. R., Chourase, M., Yadav, R., & Biswas, A. B. (2018). Status and determinants of child immunisation coverage in three South Asian countries, India, Bangladesh and Nepal: Evidence from the Demographic and Health Survey. Sri Lanka Journal of Child Health, 47(1), 56-63. https://doi.org/10.4038/sljch.v47i1.8431
Kemenkes RI. 2020. Buletin Surveilans & Imunisasi Polio Belum Berakhir. http://p2p.kemkes.go.id/buletin-surveilans-imunisasi-edisi-i-maret-2020/
Kemenkes RI. 2021. Profil Kesehatan Indonesia 2020. Jakarta Indonesia: Pusat Data dan Informasi Kemenkes RI. https://pusdatin.kemkes.go.id/resources/download/pusdatin/profil-kesehatan-indonesia/Profil-Kesehatan-Indonesia-Tahun-2020.pdf.
Luthy, K. E., Beckstrand, R. L., & Pulsipher, A. (2013). Evaluation of methods to relieve parental perceptions of vaccine-associated pain and anxiety in children: a pilot study. Journal of Pediatric Health Care, 27(5), 351-358. http://dx.doi.org/10.1016/j.pedhc.2012.02.009
Mallory, M. L., Lindesmith, L. C., & Baric, R. S. (2018). Vaccination-induced herd immunity: successes and challenges. Journal of Allergy and Clinical Immunology, 142(1), 64-66. https://doi.org/10.1016/j.jaci.2018.05.007
Mugada, V., Chandrabhotla, S., Kaja, D. S., & Machara, S. G. K. (2017). Knowledge towards childhood immunization among mothers & reasons for incomplete immunization. Journal of applied pharmaceutical science, 7(10), 157-161. http://dx.doi.org/10.7324/JAPS.2017.71023
Mursinah, M., Susanti, N., & Herna, H. (2020, July). Penolakan Vaksin di Beberapa Negara Asia dan Ancaman Penyakit yang Dapat Dicegah Dengan Imunisasi. In SINASIS (Seminar Nasional Sains) (Vol. 1, No. 1). http://proceeding.unindra.ac.id/index.php/sinasis/article/view/4009/624.
Nair, A. T., Nayar, K. R., Koya, S. F., Abraham, M., Lordson, J., Grace, C., Sreekumar, S., Chembon, P., Swarnam, K., Pillai, A. M., & Pandey, A. K. (2021). Social media, vaccine hesitancy and trust deficit in immunization programs: a qualitative enquiry in Malappuram District of Kerala, India. Health research policy and systems, 19, 1-8. https://doi.org/10.1186/s12961-021-00698-x
Nalley, J. C., & Maduka, O. (2019). Completeness and timeliness of immunization among children aged 12 to 23 months in South-South Nigeria. Journal of Community Medicine and Primary Health Care, 31(1), 22-31. https://www.ajol.info/index.php/jcmphc/article/view/185038
Odone, A., Ferrari, A., Spagnoli, F., Visciarelli, S., Shefer, A., Pasquarella, C., & Signorelli, C. (2015). Effectiveness of interventions that apply new media to improve vaccine uptake and vaccine coverage: a systematic review. Human vaccines & immunotherapeutics, 11(1), 72-82. https://doi.org/10.4161/hv.34313
Pambudi, W., Nataprawira, S. M., Atzmardina, Z., & Regina, S. (2021). Profil capaian imunisasi dasar atau lanjutan pada baduta sebelum dan selama pandemi covid-19. Jurnal Muara Medika dan Psikologi Klinis, 1(1), 17-23. https://doi.org/10.24912/jmmpk.v1i1.12054
Pinna, C., Kaewkungwal, J., Hattasingh, W., Swaddiwudhipong, W., Methakulchart, R., Moungsookjareoun, A., & Lawpoolsri, S. (2020). Evaluation of immunization services for children of migrant workers along thailand–myanmar border: Compliance with global vaccine action plan (2011–2020). Vaccines, 8(1), 68. https://doi.org/10.3390/vaccines8010068
Saeed, R., Hashmi, I., & Hashmi, S. M. I. (2021). Pakistan ranks third globally with the most unvaccinated children: is the impact of parental perception and attitude on immunization an essential contributing factor to an unsuccessful vaccination coverage?. Cureus, 13(11). https://doi.org/10.7759%2Fcureus.19751
Satriani, S., & Yuniastuti, A. (2020). Faktor Risiko Stunting Pada Balita (Studi Perbedaan Antara Dataran Rendah Dan Dataran Tinggi). J Dunia Gizi, 3(1), 32. http://ejournal.helvetia.ac.id/index.php/jdg/article/view/4666
Setiawan, M. S., & Wijayanto, A. W. (2022). Determinants of immunization status of children under two years old in Sumatera, Indonesia: A multilevel analysis of the 2020 Indonesia National Socio-Economic Survey. Vaccine, 40(12), 1821-1828. https://doi.org/10.1016/j.vaccine.2022.02.010
Siani, A. (2019). Measles outbreaks in Italy: A paradigm of the re-emergence of vaccine-preventable diseases in developed countries. Preventive medicine, 121, 99-104. https://doi.org/10.1016/j.ypmed.2019.02.011
Siramaneerat, I., & Agushybana, F. (2021). Inequalities in immunization coverage in Indonesia: a multilevel analysis. Rural and Remote Health, 21(3). https://doi.org/10.22605/RRH6348
Snider, C. J., Boualam, L., Tallis, G., Takashima, Y., Abeyasinghe, R., Lo, Y. R., Miraj, W., Lodhi, F., & Feldon, K. (2023). Concurrent outbreaks of circulating vaccine-derived poliovirus types 1 and 2 affecting the Republic of the Philippines and Malaysia, 2019–2021. Vaccine, 41, A58-A69. http://dx.doi.org/10.1016/j.medmal.2016.02.002
Tagbo, B. N., Ughasoro, M. D., & Esangbedo, D. O. (2014). Parental acceptance of inactivated polio vaccine in Southeast Nigeria: a qualitative cross-sectional interventional study. Vaccine, 32(46), 6157-6162. http://dx.doi.org/10.1016/j.vaccine.2014.08.053
Wallace, A. S., Mantel, C., Mayers, G., Mansoor, O., Gindler, J. S., & Hyde, T. B. (2014). Experiences with provider and parental attitudes and practices regarding the administration of multiple injections during infant vaccination visits: lessons for vaccine introduction. Vaccine, 32(41), 5301-5310. http://dx.doi.org/10.1016/j.vaccine.2014.07.076
Win, Z. M., Traill, T., Kyaw, Z. L., Hnin, K. T., Chit, P. T., La, T., Deshpande, A. S., Ogbuoji, O., & Mao, W. (2022). Equity assessment of childhood immunisation at national and subnational levels in Myanmar: a benefit incidence analysis. BMJ Global Health, 7(7), e007800. http://dx.doi.org/10.1136/bmjgh-2021-007800
Wong, L. P., Wong, P. F., & AbuBakar, S. (2020). Vaccine hesitancy and the resurgence of vaccine preventable diseases: the way forward for Malaysia, a Southeast Asian country. Human vaccines & immunotherapeutics, 16(7), 1511-1520. https://doi.org/10.1080/21645515.2019.1706935
Copyright (c) 2023 Ayun Sriatmi, Martini Martini, Sutopo Patria Jati, Novia Handayani, Aditya Kusumawati, Armunanto Armunanto

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
Authors retain copyright and grant the journal right of first publication with the work simultaneously licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License that allows others to share the work with an acknowledgment of the work's authorship and initial publication in this journal.
Authors are able to enter into separate, additional contractual arrangements for the non-exclusive distribution of the journal's published version of the work (e.g., post it to an institutional repository or publish it in a book), with an acknowledgment of its initial publication in this journal.
Authors are permitted to publish their work online in third parties as it can lead to wider dissemination of the work.