Human Resources Needs for Medical Records Officers at the Mataram City Health Center
Abstract
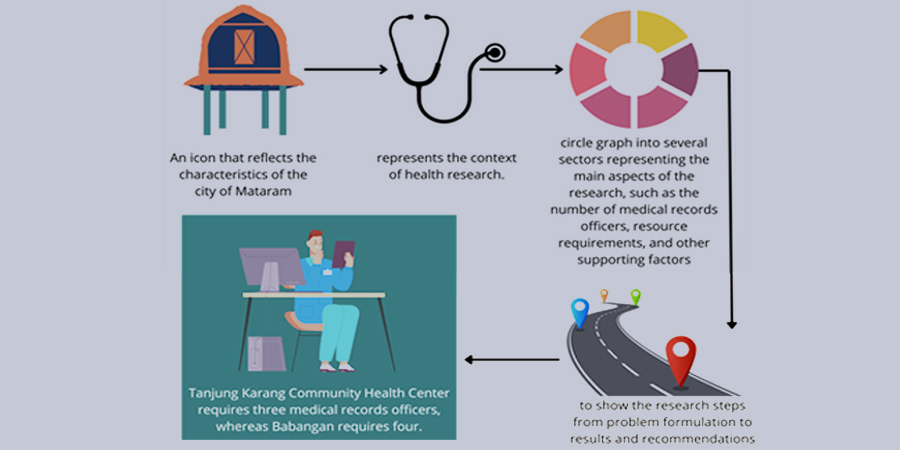
Human resources are the most important and integral part of any organization, including the health sector. Therefore, this study aimed to examine human resources needs in the medical records field, with a particular focus on the roles and responsibilities of medical records officers. The analysis was carried out to identify critical challenges faced by medical record officers in meeting health service standards and managing patient data. Secondary data were collected from a survey of workload and human resources needs for medical records in 2023. The samples were selected using the Stratified Sampling method, by dividing the population into two groups (strata) based on the accreditation levels of health centers in Mataram city. Specifically, Tanjung Karang represented the main accredited center, while Babangan was categorized as a basic accredited center. Data analysis was performed with the Workload Indicators of Staffing Need Method (WISN) to calculate labor requirements and health crew members necessary for evaluating the distribution of health worker availability. The results showed the scarcity of medical record officers, difficulties in managing patient data, as well as the need for training and skills development in line with advances in information technology within the health sector.
Downloads
References
Abid, M., & Schneider, A. B. (2023). Clinical Informatics and the Electronic Medical Record. The Surgical Clinics of North America, 103(2), 247–258. https://doi.org/10.1016/j.suc.2022.11.005
Al-Dabbagh, S. A., Sulaiman, H. M., & Abdulkarim, N. A. (2022). Workload assessment of medical doctors at primary health care centers in the Duhok governorate. Human Resources for Health, 19(Suppl 1), 117. https://doi.org/10.1186/s12960-021-00664-2
Al Bahrani, B., & Medhi, I. (2023). Copy-Pasting in Patients’ Electronic Medical Records (EMRs): Use Judiciously and With Caution. Cureus, 15(6), e40486. https://doi.org/10.7759/cureus.40486
Alghamdi, M. G. (2016a). Nursing workload: A concept analysis. Journal of Nursing Management, 24(4), 449–457. https://doi.org/10.1111/jonm.12354
Amin, M., Setyonugroho, W., &; Hidayah, N. (2021). Implementation of Electronic Medical Records: A Qualitative Study. Journal of Informatics Engineering and Information Systems, 8(1), 430–441.
Asamani, J. A., Ismaila, H., Plange, A., Ekey, V. F., Ahmed, A.-M., Chebere, M., Awoonor-Williams, J. K., & Nabyonga-Orem, J. (2021). The cost of health workforce gaps and inequitable distribution in the Ghana Health Service: an analysis towards evidence-based health workforce planning and management. Human Resources for Health, 19(1), 43. https://doi.org/10.1186/s12960-021-00590-3
Bernasinski, M., Mertes, P.-M., Carlier, M., Dupont, H., Girard, M., Gette, S., Just, B., & Malinovsky, J.-M. (2014). [Respiratory complications after transfusion]. Transfusion clinique et biologique : journal de la Societe francaise de transfusion sanguine, 21(2), 60–65. https://doi.org/10.1016/j.tracli.2014.03.002
Bowman, C. A., & Holzer, H. (2021). EMR Precharting Efficiency in Internal Medicine: A Scoping Review. Journal of Medical Education and Curricular Development, 8, 23821205211032416. https://doi.org/10.1177/23821205211032414
Bustamante Izquierdo, J. P., Puertas, E. B., Hernández Hernández, D., & Sepúlveda, H. (2023). COVID-19 and human resources for health: analysis of planning, policy responses and actions in Latin American and Caribbean countries. Human Resources for Health, 21(1), 1–19. https://doi.org/10.1186/s12960-023-00795-8
Caraballo, P. J., Bielinski, S. J., St Sauver, J. L., & Weinshilboum, R. M. (2017). Electronic Medical Record-Integrated Pharmacogenomics and Related Clinical Decision Support Concepts. Clinical Pharmacology and Therapeutics, 102(2), 254–264. https://doi.org/10.1002/cpt.707
Coates, A., Fuad, A. O., Hodgson, A., & Bourgeault, I. L. (2021). Health workforce strategies in response to major health events: a rapid scoping review with lessons learned for the response to the COVID-19 pandemic. Human Resources for Health, 19(1), 1–18. https://doi.org/10.1186/s12960-021-00698-6
de Menezes, A. A., Soares, C. L. M., Poz, M. R. D., & Pinto, I. C. M. (2022). Application of the workload indicators of staffing need method to calculate the size of the medical staff at a maternity hospital in the state of Bahia, Brazil. Human Resources for Health, 19(Suppl 1), 116. https://doi.org/10.1186/s12960-021-00660-6
Dendere, R., Slade, C., Burton-Jones, A., Sullivan, C., Staib, A., & Janda, M. (2019). Patient Portals Facilitating Engagement With Inpatient Electronic Medical Records: A Systematic Review. Journal of Medical Internet Research, 21(4), e12779. https://doi.org/10.2196/12779
Dimiri, D., Mek, N., Apini, M. T., Ali, T., Pumuye, G. T., Laka, V. J., Jogo, R., Kari, P., Deki, Mollent, O., Luo, D., Maalsen, A., Yapi, K., & Madodo, R. (2022). Estimating staffing requirements using workload indicators of staffing need at Braun District Hospital in Morobe Province, Papua New Guinea. Human Resources for Health, 19(Suppl 1), 142. https://doi.org/10.1186/s12960-021-00677-x
Doosty, F., Maleki, M. R., & Yarmohammadian, M. H. (2019). An investigation on workload indicator of staffing need: A scoping review. Journal of Education and Health Promotion, 8, 22. https://doi.org/10.4103/jehp.jehp_220_18
Evans, R. S. (2016). Electronic Health Records: Then, Now, and in the Future. Yearbook of Medical Informatics, Suppl 1(Suppl 1), S48-61. https://doi.org/10.15265/IYS-2016-s006
Fennelly, O., Cunningham, C., Grogan, L., Cronin, H., O’Shea, C., Roche, M., Lawlor, F., & O’Hare, N. (2020). Successfully implementing a national electronic health record: a rapid umbrella review. International Journal of Medical Informatics, 144, 104281. https://doi.org/10.1016/j.ijmedinf.2020.104281
Ghotane, S. G., Don-Davis, P., Kamara, D., Harper, P. R., Challacombe, S. J., & Gallagher, J. E. (2021). Needs-led human resource planning for Sierra Leone in support of oral health. Human Resources for Health, 19(1), 106. https://doi.org/10.1186/s12960-021-00623-x
Gile, P. P., van de Klundert, J., & Buljac-Samardzic, M. (2022). Human resource management in Ethiopian public hospitals. BMC Health Services Research, 22(1), 763. https://doi.org/10.1186/s12913-022-08046-7
Greysen, S. R., Magan, Y., Rosenthal, J., Jacolbia, R., Auerbach, A. D., & Harrison, J. D. (2020). Patient Recommendations to Improve the Implementation of and Engagement With Portals in Acute Care: Hospital-Based Qualitative Study. Journal of Medical Internet Research, 22(1), e13337. https://doi.org/10.2196/13337
Hasanah, F. N., Okiyanti, P., & Sonia, D. (2022). Perhitungan Kebutuhan SDMK dengan Metode ABK-KES di Klinik Pratama Green Care Kota Bandung. Jurnal Wiyata: Penelitian Sains dan Kesehatan, 9(1), 33-42. http://dx.doi.org/10.56710/wiyata.v9i1.517
Hasrawati, H., Ahmad, L. O. I., & Hartoyo, A. M. (2020). Analisis Kebutuhan Tenaga Perawat Berdasarkan Beban Kerja Dengan Menggunakan Metode Analisis Beban Kerja Kesehatan (ABK KES) di Instalasi Rawat Inap RSU Aliyah Kota Kendari Tahun 2020. Journal of Health Policy Administration Halu Oleo University, 1(3). http://dx.doi.org/10.37887/jakk.v1i3.38089
Henderson, J., Bouck, Z., Holleman, R., Chu, C., Klamerus, M. L., Santiago, R., Bhatia, R. S., & Kerr, E. A. (2020). Comparison of Payment Changes and Choosing Wisely Recommendations for Use of Low-Value Laboratory Tests in the United States and Canada. JAMA Internal Medicine, 180(4), 524–531. https://doi.org/10.1001/jamainternmed.2019.7143
Jagetia, G. C. (2022). Genotoxic effects of electromagnetic field radiations from mobile phones. Environmental Research, 212(Pt D), 113321. https://doi.org/10.1016/j.envres.2022.113321
Janett, R. S., & Yeracaris, P. P. (2020). Electronic medical records in the american health system: Challenges and lessons learned. Ciencia e Saude Coletiva, 25(4), 1293–1304. https://doi.org/10.1590/1413-81232020254.28922019
Jing, Q., Xing, Y., Duan, M., Guo, P., Cai, W., Gao, Q., Gao, R., Ji, L., & Lu, J. (2022). Study on the Rehabilitation Therapist Estimation Under Institutional Perspective by Applying the Workload Indicators of Staffing Needs in the Aging Context. Frontiers in Public Health, 10, 929675. https://doi.org/10.3389/fpubh.2022.929675
Kiri, V. A., & Ojule, A. C. (2020). Electronic medical record systems: A pathway to sustainable public health insurance schemes in sub-Saharan Africa. The Nigerian Postgraduate Medical Journal, 27(1), 1–7. https://doi.org/10.4103/npmj.npmj_141_19
Köppen, J., Hartl, K., & Maier, C. B. (2021). Health workforce response to Covid-19: What pandemic preparedness planning and action at the federal and state levels in Germany?: Germany’s health workforce responses to Covid-19. The International Journal of Health Planning and Management, 36(S1), 71–91. https://doi.org/10.1002/hpm.3146
Lestari, D. P., & Harno. (2018). Calculation of Medical Record Personnel Needs with Health Workload Analysis (HWA) at Sentolo 1 Health Center. https://api.semanticscholar.org/CorpusID:146004848
McVey, C. (2023). Telenursing: A Concept Analysis. Computers, Informatics, Nursing : CIN, 41(5), 275–280. https://doi.org/10.1097/CIN.0000000000000973
Mills, S. (2019). Electronic Health Records and Use of Clinical Decision Support. Critical Care Nursing Clinics of North America, 31(2), 125–131. https://doi.org/10.1016/j.cnc.2019.02.006
Moriyama, A. S., Dos Santos Forseto, A., Pereira, N. C., Ribeiro, A. C., de Almeida, M. C., Figueras-Roca, M., Casaroli-Marano, R. P., Mehta, J. S., & Hofling-Lima, A. L. (2022). Trends in Corneal Transplantation in a Tertiary Hospital in Brazil. Cornea, 41(7), 857–866. https://doi.org/10.1097/ICO.0000000000002801
Namaganda, G. N., Whitright, A., & Maniple, E. B. (2022). Lessons learned from implementation of the Workload Indicator of Staffing Need (WISN) methodology: an international Delphi study of expert users. Human Resources for Health, 19(Suppl 1), 138. https://doi.org/10.1186/s12960-021-00675-z
Nazhifah, N., Yustika, I. A., & Hidayati, M. (2021). Analisis Kebutuhan SDM Petugas Rekam Medis dengan Menggunakan Metode Analisis Beban Kerja Kesehatan (ABK-Kes). Cerdika: Jurnal Ilmiah Indonesia. 1(8), 1021-1028. https://doi.org/10.59141/cerdika.v1i8.169
Nelson, C., Lurie, N., Wasserman, J., & Zakowski, S. (2007). Conceptualizing and defining public health emergency preparedness. In American journal of public health: Vol. 97 Suppl 1 (Issue Suppl 1, pp. S9-11). https://doi.org/10.2105/AJPH.2007.114496
Nguyen, T. T. H., Phung, H. T., & Bui, A. T. M. (2022). Applying the workload indicators of staffing needs method in nursing health workforce planning: evidences from four hospitals in Vietnam. Human Resources for Health, 19(Suppl 1), 124. https://doi.org/10.1186/s12960-021-00668-y
O’Byrne, L., Gavin, B., & McNicholas, F. (2020). Medical students and COVID-19: the need for pandemic preparedness. Journal of Medical Ethics, 46(9), 623–626. https://doi.org/10.1136/medethics-2020-106353
Pan American Health Organization. (2022). The COVID-19 HEalth caRe wOrkErS Study (HEROES).
Pantelakos, S., & Agrogiannis, G. (2023). Comparative Analysis of Three Workload Measurement Methodologies in Surgical Pathology: Conclusions and Implications on Public Health Care and Costing of Pathology Services. American Journal of Clinical Pathology, 160(2), 185–193. https://doi.org/10.1093/ajcp/aqad030
Parulian Gultom, S., & Sopian. (2019). Analisis Kebutuhan Tenaga Rekam Medis Berdasarkan Beban Kerja Di Bagian Pelaporan Rumah Sakit Khusus Ginjal Rasyida Tahun 2018. Jurnal Ilmiah Perekam Dan Informasi Kesehatan Imelda (JIPIKI), 3(2), 486–492. https://doi.org/10.52943/jipiki.v3i2.67
Putri, C. A., & Hidayati, M. (2021). Analisis Kebutuhan Sumber Daya Manusia Petugas Rekam Medis Dengan Menggunakan Metode Analisis Beban Kerja Kesehatan (Abk-Kes). Jurnal Manajemen Kesehatan Yayasan RS. Dr. Soetomo, 7(2), 257-266. http://dx.doi.org/10.29241/jmk.v7i2.637
Rashid, M. U., Alomari, M., Afraz, S., & Erim, T. (2022). EMR and ESD: Indications, techniques and results. Surgical Oncology, 43, 101742. https://doi.org/10.1016/j.suronc.2022.101742
Safer, J. D., Coleman, E., Feldman, J., Garofalo, R., Hembree, W., Radix, A., & Sevelius, J. (2016). Barriers to healthcare for transgender individuals. Current Opinion in Endocrinology, Diabetes, and Obesity, 23(2), 168–171. https://doi.org/10.1097/MED.0000000000000227
Saiful, S., Muchlis, N., & Patimah, S. (2022). Analisis perencanaan sumber daya manusia (SDM) kesehatan dengan metode workload indicators of staffing need (WISN) di RSUD Undata Palu Sulawesi Tengah Tahun 2022. Journal of Muslim Community Health (JMCH) 2022, 3(3), 110–119. https://doi.org/10.52103/jmch.v3i3.993
Suryanto, H. (2020). Workload Analysis and Human Resource Needs Record Officer Workload Analysis and Human Resource Needs Medical Record Officer of Adan-adan Health Center, Kediri Regency. Journal of Medical Records and Health Information, March 2020. https://doi.org/10.31983/jrmik.v3i1.5514
Swiger, P. A., Vance, D. E., & Patrician, P. A. (2016). Nursing workload in the acute-care setting: A concept analysis of nursing workload. Nursing Outlook, 64(3), 244–254. https://doi.org/10.1016/j.outlook.2016.01.003
Tripković, K., Šantrić Milićević, M., Mandić Miladinović, M., Kovačević, L., Bjegović Mikanović, V., & Vuković, D. (2022). Implementation of the Workload Indicators of Staffing Need (WISN) Method in Determining Staff Requirements in Public Health Laboratories in Serbia. Disaster Medicine and Public Health Preparedness, 16(1), 71–79. https://doi.org/10.1017/dmp.2020.133
Walton-Roberts, M. (2022). The ethics of recruiting foreign-trained healthcare workers. Healthcare Management Forum, 35(4), 248–251. https://doi.org/10.1177/08404704221095129
Wardanis, D. T. (2018). Analisis Beban Kerja Tenaga Rekam Medis Rumah Sakit Bedah SurabayaMenggunakan Metode FTE. Jurnal Administrasi Kesehatan Indonesia, 6(1), 53. https://doi.org/10.20473/jaki.v6i1.2018.53-60
WHO. (2021). Impact of COVID-19 on human resources for health and policy response: the case of Plurinational State of Bolivia, Chile, Colombia, Ecuador and Peru. Overview of findings from five Latin American countries. https://apps.who.int/iris/bitstream/handle/10665/350640/9789240039001-eng.pdf
Williams, G. A., Jacob, G., Rakovac, I., Scotter, C., & Wismar, M. (2020). Health professional mobility in the WHO European Region and the WHO Global Code of Practice: data from the joint OECD/EUROSTAT/WHO-Europe questionnaire. European Journal of Public Health, 30(Suppl_4), iv5–iv11. https://doi.org/10.1093/eurpub/ckaa124
Copyright (c) 2023 Syamsuriansyah Syamsuriansyah, Hizriyansyah Hizriyansyah, Nik Azliza Nik Ariffin, Rizal Pratama Adi Putra

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
Authors retain copyright and grant the journal right of first publication with the work simultaneously licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License that allows others to share the work with an acknowledgment of the work's authorship and initial publication in this journal.
Authors are able to enter into separate, additional contractual arrangements for the non-exclusive distribution of the journal's published version of the work (e.g., post it to an institutional repository or publish it in a book), with an acknowledgment of its initial publication in this journal.
Authors are permitted to publish their work online in third parties as it can lead to wider dissemination of the work.






