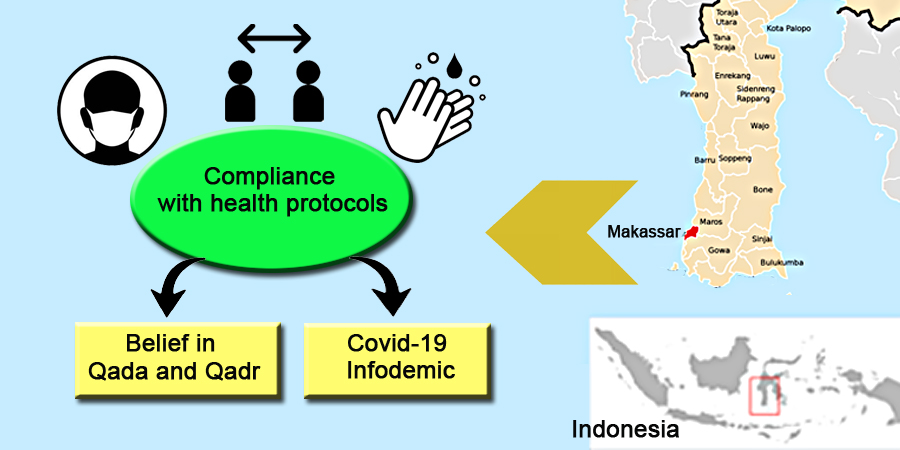
Islamic Faith Belief and Infodemic Toward Society's Compliance With Covid-19 Health Protocols
Abstract
The implementation of health protocols during Covid-19 pandemic is very important to the prevention of virus transmission, but it had not been implemented optimally. Therefore, this study aimed to analyze the contribution of provisions in Islamic teachings and Infodemic to compliance with health protocols. The quantitative method was adopted with an observational study approach involving a total of 421 people. This sample was selected using the criteria of being Muslim, at least 18 years old, and willing to fill out a questionnaire online using the Google form. The results showed that the contribution of Islamic teachings in the form of Qada and Qadr belief and Covid-19 Infodemic had a positive effect on compliance with implementing the health protocols. Furthermore, the contribution of belief in Islamic teachings and Covid-19 Infodemic had a simultaneous positive effect on compliance with implementing health protocols. This study proved that religious and spiritual approaches can effectively increase community compliance in adhering to public health efforts.
Downloads
References
Ahmad, A. R., & Murad, H. R. (2020). The impact of social media on panic during the COVID-19 pandemic in Iraqi Kurdistan: online questionnaire study. Journal of medical Internet research, 22(5), e19556. https://doi.org/10.2196/19556
Al-Asqalani, I. H. (2020). Kitab Wabah dan Taun dalam Islam. Jakarta: Turos Pustaka.
Apuke, O. D., & Omar, B. (2021). Fake news and COVID-19: modelling the predictors of fake news sharing among social media users. Telematics and Informatics, 56, 101475. https://doi.org/10.1016/j.tele.2020.101475
Chen, J. Y., Fox, S. A., Cantrell, C. H., Stockdale, S. E., & Kagawa-Singer, M. (2006). Health Disparities And Prevention: Racial/ethnic Barriers To Flu Vaccinations. Journal of Community Health, 32(1), 5–20. https://doi.org/10.1007/s10900-006-9031-7
Cherniak, A. D., Pirutinsky, S., & Rosmarin, D. H. (2023). Religious Beliefs, Trust In Public Figures, And Adherence to COVID-19 Health Guidelines among American Orthodox and Non-Orthodox Jews. Journal of religion and health, 62(1), 355-372. https://doi.org/10.1007/s10943-022-01718-y
Dinas Kesehatan Provinsi Sulawesi Selatan. (2021). Data Pantauan Covid-19 di Sulawesi Selatan.
Dubey, S., Biswas, P., Ghosh, R., Chatterjee, S., Dubey, M. J., Chatterjee, S., Lahiri, D., & Lavie, C. J. (2020). Psychosocial impact of COVID-19. Diabetes and Metabolic Syndrome: Clinical Research and Reviews, 14(5), 779–788. https://doi.org/10.1016/j.dsx.2020.05.035
Gagneux-Brunon, A., Detoc, M., Bruel, S., Tardy, B., Rozaire, O., Frappe, P., & Botelho- Nevers, E. (2021). Intention to get vaccinations against COVID-19 in French healthcare workers during the first pandemic wave: a cross-sectional survey. Journal of Hospital Infection, 108, 168–173. https://doi.org/https://doi.org/10.1016/j.jhin.2020.11.020
Gan, S. K. E., Wong, S. W. Y., & Jiao, P. D. (2023). Religiosity, theism, perceived social support, resilience, and well-being of university undergraduate students in Singapore during the COVID-19 pandemic. International Journal of Environmental Research and Public Health, 20(4), 3620. https://doi.org/10.3390/ijerph20043620
Geldsetzer, P. (2020). Knowledge and perceptions of COVID-19 among the general public in the United States and the United Kingdom: a cross-sectional online survey. Annals of internal medicine, 173(2), 157-160. https://doi.org/10.7326/M20-0912
Ho, H. Y., Chen, Y. L., & Yen, C. F. (2020). Different impacts of COVID-19-related information sources on public worry: An online survey through social media. Internet interventions, 22, 100350. https://doi.org/10.1016/j.invent.2020.100350
Huda, M., Sudrajat, A., Muhamat, R., Mat Teh, K. S., & Jalal, B. (2019). Strengthening divine values for self-regulation in religiosity: insights from Tawakkul (trust in God). International Journal of Ethics and Systems, 35(3), 323-344. https://doi.org/10.1108/IJOES-02-2018-0025
Ioannidis, J. P. A. (2020). Coronavirus disease 2019: The harms of exaggerated information and non-evidence-based measures. European Journal of Clinical Investigation, 50(4), 1–5. https://doi.org/10.1111/eci.13222
Ioannidis, J. P. A. (2020). Coronavirus disease 2019: The harms of exaggerated information and non-evidence-based measures. European Journal of Clinical Investigation, 50(4), 1–5. https://doi.org/10.1111/eci.13222
Isiko, A. P. (2020). Religious construction of disease: An exploratory appraisal of religious responses to the COVID-19 pandemic in Uganda. Journal of African Studies and Development, 12(3), 77–96. https://doi.org/10.5897/JASD2020.0573
Jolley, D., & Douglas, K. M. (2017). Prevention is better than cure: Addressing anti‐ vaccine conspiracy theories. Journal of Applied Social Psychology, 47(8), 459–469. https://doi.org/10.1111/jasp.12453
Juditha, C. (2020). Perilaku Masyarakat Terkait Penyebaran Hoaks Covid-19 People Behavior Related To The Spread Of Covid-19’s Hoax. Jurnal Pekommas, 5(2), 105–116. https://doi.org/10.30818/jpkm.2020.2050201
Khan, Y. H., Mallhi, T. H., Alotaibi, N. H., Alzarea, A. I., Alanazi, A. S., Tanveer, N., & Hashmi, F. K. (2020). Threat of COVID-19 vaccine hesitancy in Pakistan: the need for measures to neutralize misleading narratives. The American Journal of Tropical Medicine and Hygiene, 103(2), 603–604. https://doi.org/10.4269%2Fajtmh.20-0654
Komisi Pemilihan Umum Sulawesi Selatan. (2015). KPU Tetapkan DPT Pilgub Sulsel 6.022.087 Jiwa.
Kowalczyk, O., Roszkowski, K., Montane, X., Pawliszak, W., Tylkowski, B., & Bajek, A. (2020). Religion and faith perception in a pandemic of COVID-19. Journal of religion and health, 59, 2671-2677. https://doi.org/10.1007/s10943-020-01088-3
Kwok, K. O., Li, K.-K., Wei, W. I., Tang, A., Wong, S. Y. S., & Lee, S. S. (2021). Influenza vaccine uptake, COVID-19 vaccination intention and vaccine hesitancy among nurses: A survey. International Journal of Nursing Studies, 114, 103854. https://doi.org/10.1016/j.ijnurstu.2020.103854
Lazarus, J. V, Ratzan, S. C., Palayew, A., Gostin, L. O., Larson, H. J., Rabin, K., Kimball, S., & El-Mohandes, A. (2021). A global survey of potential acceptance of a COVID-19 vaccine. Nature Medicine, 27(2), 225–228. https://doi.org/10.1038/s41591-020-1124-9
Lin, C., Tu, P., & Beitsch, L. M. (2021). Confidence and Receptivity for COVID-19 Vaccines: A Rapid Systematic Review. Vaccines, 9(1), 16. https://doi.org/10.3390/vaccines9010016
Lin, C. Y., Broström, A., Griffiths, M. D., & Pakpour, A. H. (2020). Investigating mediated effects of fear of COVID-19 and COVID-19 misunderstanding in the association between problematic social media use, psychological distress, and insomnia. Internet interventions, 21, 100345. https://doi.org/10.1016/j.invent.2020.100345
Lin, F., Chen, X., & Cheng, E. W. (2022). Contextualized impacts of an infodemic on vaccine hesitancy: The moderating role of socioeconomic and cultural factors. Information Processing & Management, 59(5), 103013. https://doi.org/10.1016/j.ipm.2022.103013
López-García, X., Costa-Sánchez, C., & Vizoso, Á. (2021). Journalistic fact-checking of information in pandemic: Stakeholders, hoaxes, and strategies to fight disinformation during the COVID-19 crisis in Spain. International journal of environmental research and public health, 18(3), 1227. https://doi.org/10.3390/ijerph18031227
Luk, T. T., Zhao, S., Wu, Y., Wong, J. Y. H., Wang, M. P., & Lam, T. H. (2021). Prevalence and determinants of SARS-CoV-2 vaccine hesitancy in Hong Kong: A population-based survey. Vaccine, 39(27), 3602-3607. https://doi.org/10.1016/j.vaccine.2021.05.036
Machida, M., Nakamura, I., Kojima, T., Saito, R., Nakaya, T., Hanibuchi, T., Takamiya, T., Odagiri, Y., Fukushima, N., Kikuchi, H., Amagasa, S., Watanabe, H., & Inoue, S. (2021). Acceptance of a COVID-19 Vaccine in Japan during the COVID-19 Pandemic. Vaccines, 9(3), 210. https://doi.org/10.3390/vaccines9030210
Masip, P., Aran-Ramspott, S., Ruiz-Caballero, C., Suau, J., Almenar, E., & Puertas-Graell, D. (2020). Consumo informativo y cobertura mediática durante el confinamiento por el Covid-19: sobreinformación, sesgo ideológico y sensacionalismo. El Profesional de La Información, 29(3), 1–12. https://doi.org/10.3145/epi.2020.may.12
Mills, M. C., & Salisbury, D. (2021). The challenges of distributing COVID-19 vaccinations. EClinicalMedicine, 31. https://doi.org/10.1016/j.eclinm.2020.100674
Moon, M. J. (2020). Fighting COVID‐19 with agility, transparency, and participation: Wicked policy problems and new governance challenges. Public administration review, 80(4), 651-656. https://doi.org/10.1111/puar.13214
Murphy, J., Vallières, F., Bentall, R. P., Shevlin, M., McBride, O., Hartman, T. K., McKay, R., Bennett, K., Mason, L., & Gibson-Miller, J. (2021). Psychological characteristics associated with COVID-19 vaccine hesitancy and resistance in Ireland and the United Kingdom. Nature Communications, 12(1), 1–15. https://doi.org/10.1038/s41467-020-20226-9
Nelson, L. M., Simard, J. F., Oluyomi, A., Nava, V., Rosas, L. G., Bondy, M., & Linos, E. (2020). US public concerns about the COVID-19 pandemic from results of a survey given via social media. JAMA internal medicine, 180(7), 1020-1022. http://www.doi.org/10.1001/jamainternmed.2020.1369
Paul, E., Steptoe, A., & Fancourt, D. (2021). Attitudes towards vaccines and intention to vaccinate against COVID-19: Implications for public health communications. The Lancet Regional Health - Europe, 1, 100012. https://doi.org/https://doi.org/10.1016/j.lanepe.2020.100012
Plohl, N., & Musil, B. (2021). Modeling compliance with COVID-19 prevention guidelines : the critical role of trust in science Modeling compliance with COVID-19 prevention guidelines : the critical role of trust in science. Psychology, Health & Medicine, 26(1), 1–12. https://doi.org/10.1080/13548506.2020.1772988
Rahimi, F., & Abadi, A. T. B. (2021). Implications of the Emergence of a New Variant of SARS-CoV-2, VUI-202012/01. Archives of Medical Research. https://doi.org/10.1016/j.arcmed.2021.01.001
Ramly, R. M. (2022). Theological Issues of Pandemic Covid-19 in Malaysia : The Views of the Muslims Theologians. Jurnal THEOLOGIA, 33(1), 1–18. https://doi.org/10.21580/teo.2022.33.1.11521
Raquel, C. P., Ribeiro, K. G., Alencar, N. E. S., de Souza, D. F. O., Barreto, I. C. de H. C., & de Andrade, L. O. M. (2022). Scientific ways to confront covid-19 fake news. Saude e Sociedade, 31(4), 1–16. https://doi.org/10.1590/S0104-12902022210601en
Rizky, M. H. K. (2022). Corona Virus Disease 19 On Islamic Theological Reflection. Sophist: Jurnal Sosial Politik Kajian Islam dan Tafsir, 4(1), 21-41. https://doi.org/10.20414/sophist.v4i1.62
Robertson, E., Reeve, K. S., Niedzwiedz, C. L., Moore, J., Blake, M., Green, M., Katikireddi, S. V., & Benzeval, M. J. (2021). Predictors of COVID-19 vaccine hesitancy in the UK household longitudinal study. Brain, behavior, and immunity, 94, 41-50. https://doi.org/10.1016/j.bbi.2021.03.008
Romer, D., & Jamieson, K. H. (2020). Conspiracy theories as barriers to controlling the spread of COVID-19 in the US. Social Science & Medicine, 263, 113356. https://doi.org/10.1016/j.socscimed.2020.113356
Sahoo, B. P., & Patel, A. B. (2021). Social stigma in time of COVID-19 pandemic: evidence from India. International Journal of Sociology and Social Policy, 41(11/12), 1170-1182. https://doi.org/10.1108/IJSSP-01-2021-0012
Schwarzinger, M., Watson, V., Arwidson, P., Alla, F., & Luchini, S. (2021). COVID-19 vaccine hesitancy in a representative working-age population in France: a survey experiment based on vaccine characteristics. The Lancet Public Health. https://doi.org/10.1016/S2468-2667(21)00012-8
Simanjuntak, D. R., Napitupulu, T. M., Wele, A. M., & Yanie, R. (2020). Gambaran kepatuhan masyarakat menerapkan protokol kesehatan Covid-19 di tempat umum periode September 2020 di DKI Jakarta.
South Sulawesi Provincial Government, 2022. Kasus Covid-19 Melonjak, BOR ICU dan Isolasi di Sulsel.Terkendali. Access on 13 February 2022. https://humas.sulselprov.go.id/index.php/tag/covid-19/
Sukawana, I. W., & Sukarja, I. M. (2021). Gambaran Kepatuhan Masyarakat Mawang Kelod Dalam Menerapkan Protokol Pencegahan Covid-19 di Tempat Umum Bulan September 2020. Community Publ Nurs, 9(2), 204–210. https://doi.org/10.30818/jpkm.2020.2050201
Tambo, E., Djuikoue, I. C., Tazemda, G. K., Fotsing, M. F., & Zhou, X. N. (2021). Early stage risk communication and community engagement (RCCE) strategies and measures against the coronavirus disease 2019 (COVID-19) pandemic crisis. Global Health Journal, 5(1), 44-50. https://doi.org/10.1016/j.glohj.2021.02.009
Tram, K. H., Saeed, S., Bradley, C., Fox, B., Eshun-Wilson, I., Mody, A., & Geng, E. (2022). Deliberation, dissent, and distrust: understanding distinct drivers of coronavirus disease 2019 vaccine hesitancy in the United States. Clinical Infectious Diseases, 74(8), 1429-1441. https://doi.org/10.1093/cid/ciab633
Wang, D., Marmo-Roman, S., Krase, K., & Phanord, L. (2021). Compliance with preventative measures during the COVID-19 pandemic in the USA and Canada: Results from an online survey. Social Work in Health Care, 1–16. https://doi.org/10.1080/00981389.2020.1871157
Yang, F., Li, X., Su, X., Xiao, T., Wang, Y., Hu, P., Li, H., Guan, J., Tian, H., Wang, P., & Wang, W. (2021). A study on willingness and influencing factors to receive COVID-19 vaccination among Qingdao residents. Human Vaccines & Immunotherapeutics, 17(2), 408–413. https://doi.org/10.1080/21645515.2020.1817712
Yao, H. (2020). The more exposure to media information about COVID-19, the more distressed you will feel. Brain, behavior, and immunity, 87, 167. https://doi.org/10.1016%2Fj.bbi.2020.05.031
Zhang, Y., Luo, X., & Ma, Z. F. (2021). Willingness of the general population to accept and pay for COVID-19 vaccination during the early stages of COVID-19 pandemic: a nationally representative survey in mainland China. Human Vaccines & Immunotherapeutics, 1–6. https://doi.org/10.1080/21645515.2020.1847585
Zielinski, C. (2021). Infodemics and infodemiology: A short history, a long future. Revista Panamericana de Salud Publica/Pan American Journal of Public Health, 45, 1–8. https://doi.org/10.26633/RPSP.2021.40
Copyright (c) 2023 Sitti Raodhah, Azman Arsyad

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
Authors retain copyright and grant the journal right of first publication with the work simultaneously licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License that allows others to share the work with an acknowledgment of the work's authorship and initial publication in this journal.
Authors are able to enter into separate, additional contractual arrangements for the non-exclusive distribution of the journal's published version of the work (e.g., post it to an institutional repository or publish it in a book), with an acknowledgment of its initial publication in this journal.
Authors are permitted to publish their work online in third parties as it can lead to wider dissemination of the work.






