Fluor Albus Characteristics Associated with Sexually Transmitted Infection (STI) in Makassar Pregnant Women
Abstract
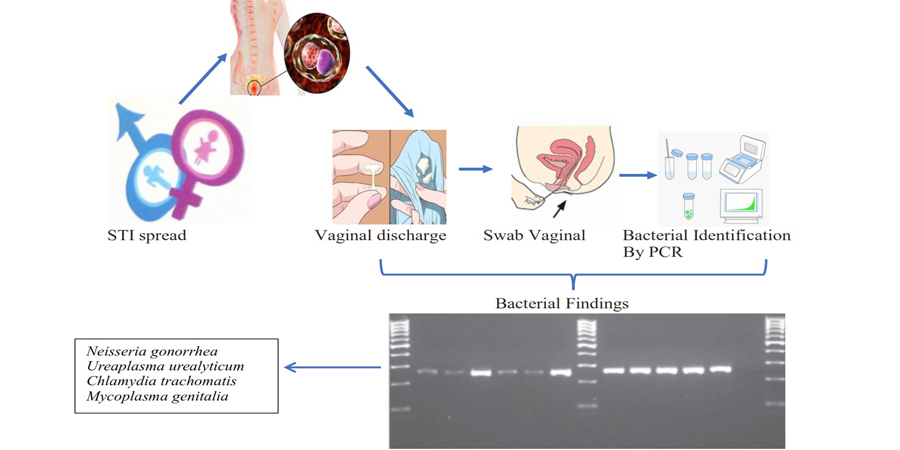
Sexually Transmitted Infection (STI) is a common condition with increased prevalence among pregnant women and can negatively affect the fetus. According to WHO, a total of 374 million new cases of STI are projected to occur in 2020, including gonorrhea (82 million), syphilis (7.1 million), and trichomoniasis (156 million). Therefore, this study aimed to determine the relationship between the characteristics of vaginal discharge (fluor albus) in pregnant women and STI. The descriptive method was used with a cross-sectional design, and the procedures were conducted in May 2023. The sample population comprised all pregnant women with ANC in Makassar during the study period. Vaginal swabs were obtained from 127 pregnant women who were willing to participate and had vaginal discharge. The results showed that 53 participants reported having physiological flour albus, while 74 had pathological symptoms. Itching and odor were reported to be the most common clinical signs associated with patients' abnormal vaginal discharge, followed by itching, pain, and odor. Furthermore, a significantly high prevalence of the condition was observed among pregnant women aged 20-30 years. Based on the results, the predominant symptom of fluor albus was itching and odor when combined with microorganisms that caused STI. Several pregnant women with clinical complaints also had microorganisms apart from those associated with STI. These results indicated the pressing need to develop additional testing in pregnant women with fluor albus, particularly those with concomitant symptoms.
Downloads
References
Abu-Raya, B., Michalski, C., Sadarangani, M., & Lavoie, P. M. (2020). Maternal Immunological Adaptation During Normal Pregnancy. Frontiers in Immunology, 11. https://doi.org/10.3389/fimmu.2020.575197
Aduloju, O. P., Akintayo, A. A., & Aduloju, T. (2019). Prevalence of bacterial vaginosis in pregnancy in a tertiary health institution, south western Nigeria. The Pan African Medical Journal, 33. https://doi.org/10.11604%2Fpamj.2019.33.9.17926
Almubarak, S. S., Alsofyani, A. H., Alhbabi, Z., Almahboob, G. S., Alodail, M., Alaswad, F., & Alfayez, M. (2020). Increased vaginal discharge during pregnancy: prevalence, causes, and associated symptoms. Age, 21(46), 4-5. http://dx.doi.org/10.24911/IJMDC.51-1578948957
Amare. (2021). 2020 STD Prevention Conference September 14–24, 2020: Erratum. Sexually Transmitted Diseases, 48(2), e34–e34. https://doi.org/10.1097/OLQ.0000000000001346
Bosaeus, M., Andersson-Hall, U., Andersson, L., Karlsson, T., Ellegård, L., & Holmäng, A. (2020). Body Composition During Pregnancy: Longitudinal Changes and Method Comparisons. Reproductive Sciences, 27(7), 1477–1489. https://doi.org/10.1007/s43032-020-00141-6
Centers for Disease Control and Prevention (2022). STD Facts - STDs & Pregnancy. https://www.cdc.gov/std/pregnancy/stdfact-pregnancy.htm
Centers for Disease Control and Prevention (2023). STDs & Infertility. https://www.cdc.gov/std/infertility/default.htm
Contini, C., Rotondo, J. C., Magagnoli, F., Maritati, M., Seraceni, S., Graziano, A., Poggi, A., Capucci, R., Vesce, F., Tognon, M., & Martini, F. (2019). Investigation on silent bacterial infections in specimens from pregnant women affected by spontaneous miscarriage. Journal of Cellular Physiology, 234(1), 100–107. https://doi.org/10.1002/jcp.26952
Garcia, M. R., Leslie, S. W., & Wray, A. A. (2023). Sexually transmitted infections. In StatPearls [Internet]. StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK560808/
Gupta, N. K., & Bowman, C. A. (2012). Managing Sexually Transmitted Infections in Pregnant Women. Women’s Health, 8(3), 313–321. https://doi.org/10.2217/WHE.12.16
Isara, A., & Baldeh, A. K. (2021). Prevalence of sexually transmitted infections among pregnant women attending antenatal clinics in West Coast Region of The Gambia. African Health Sciences, 21(2), 585–592. https://doi.org/10.4314/ahs.v21i2.13
Jonduo, M. E., Vallely, L. M., Wand, H., Sweeney, E. L., Egli-Gany, D., Kaldor, J., Vallely, A. J., & Low, N. (2022). Adverse pregnancy and birth outcomes associated with Mycoplasma hominis, Ureaplasma urealyticum and Ureaplasma parvum : a systematic review and meta-analysis. BMJ Open, 12(8), e062990. https://doi.org/10.1136/bmjopen-2022-062990
Kementrian Kesehatan (2020). Laporan Perkembangan HIV AIDS & Penyakit Infeksi Menular Seksual (PIMS) Triwulan III Tahun 2020. https://siha.kemkes.go.id/
Khaskheli, M., Baloch, S., Baloch, A. S., & Shah, S. G. S. (2021). Vaginal discharge during pregnancy and associated adverse maternal and perinatal outcomes. Pakistan journal of medical sciences, 37(5), 1302. https://doi.org/10.12669%2Fpjms.37.5.4187
Kokkayil, P., & Dhawan, B. (2015). Ureaplasma: Current perspectives. Indian Journal of Medical Microbiology, 33(2), 205–214. https://doi.org/10.4103/0255-0857.154850
Lee, S. R., Chung, J. M., & Kim, Y. G. (2007). Rapid One Step Detection of Pathogenic Bacteria in Urine with Sexually Transmitted Disease (STD) and Prostatitis Patient by Multiplex PCR Assay (mPCR). In The Microbiological Society of Korea (Vol. 45, Issue 5). http://ncbi.nlm.nhi.gov/BLAST
Liu, T., Lai, S. Y., Zhou, W., Liu, Y. L., Chen, S. S., & Jiang, Y. M. (2022). Analysis of Ureaplasma urealyticum, Chlamydia trachomatis, Mycoplasma genitalium and Neisseria gonorrhoeae infections among obstetrics and gynecological outpatients in southwest China: a retrospective study. BMC Infectious Diseases, 22(1), 283. https://doi.org/10.1186/s12879-021-06966-z
Luján, A., Fili, S., & Damiani, M. T. (2016). Female Infertility Associated to Chlamydia trachomatis Infection. In Genital Infections and Infertility. InTech. https://doi.org/10.5772/62462
Olaleye, A. O., Babah, O. A., Osuagwu, C. S., Ogunsola, F. T., & Afolabi, B. B. (2020). Sexually transmitted infections in pregnancy – An update on Chlamydia trachomatis and Neisseria gonorrhoeae. European Journal of Obstetrics & Gynecology and Reproductive Biology, 255, 1–12. https://doi.org/10.1016/j.ejogrb.2020.10.002
Olcu, M., Atalay, M. A., & Percin Renders, D. (2022). Development of multiplex PCR panel for detection of anaerobic bacteria in clinical samples. Anaerobe, 76, 102611. https://doi.org/10.1016/j.anaerobe.2022.102611
Pillay, J., Moore, A., Rahman, P., Lewin, G., Reynolds, D., Riva, J., Thériault, G., Thombs, B., Wilson, B., Robinson, J., Ramdyal, A., Cadieux, G., Featherstone, R., Burchell, A. N., Dillon, J.-A., Singh, A., Wong, T., Doull, M., Traversy, G., Hartling, L. (2018). Screening for chlamydia and/or gonorrhea in primary health care: protocol for systematic review. Systematic Reviews, 7(1), 248. https://doi.org/10.1186/s13643-018-0904-5
Prasad, D., Parween, S., Kumari, K., & Singh, N. (2021). Prevalence, Etiology, and Associated Symptoms of Vaginal Discharge During Pregnancy in Women Seen in a Tertiary Care Hospital in Bihar. Cureus, 13(1), e12700-e12700. https://doi.org/10.7759/cureus.12700
Sawant, L. D. (2017). Sexually Transmitted Infections in Pregnancy. International Journal of Pregnancy & Child Birth, 2(6). https://doi.org/10.15406/ipcb.2017.02.00044
Smith, M. (2021). Validating Real-Time Polymerase Chain Reaction (PCR) Assays. Encyclopedia of Virology, 35–44. https://doi.org/10.1016/b978-0-12-814515-9.00053-9
Tanwar, R., Sarda, S., Agarwal, S., & Dubey, S. (2022). Prevalence of Sexually Transmitted Infection in Pregnancy at a Tertiary Care Center of Central India: An Observational Study. Journal of South Asian Federation of Obstetrics and Gynaecology, 14(2), 128–131. https://doi.org/10.5005/jp-journals-10006-2039
Tuddenham, S., Hamill, M. M., & Ghanem, K. G. (2022). Diagnosis and Treatment of Sexually Transmitted Infections. JAMA, 327(2), 161. https://doi.org/10.1001/jama.2021.23487
Warr, A. J., Pintye, J., Kinuthia, J., Drake, A. L., Unger, J. A., McClelland, R. S., Matemo, D., Osborn, L., & John-Stewart, G. (2019). Sexually transmitted infections during pregnancy and subsequent risk of stillbirth and infant mortality in Kenya: a prospective study. Sexually Transmitted Infections, 95(1), 60–66. https://doi.org/10.1136/sextrans-2018-053597
Whelan, J., Eeuwijk, J., Bunge, E., & Beck, E. (2021). Systematic Literature Review and Quantitative Analysis of Health Problems Associated with Sexually Transmitted Neisseria gonorrhoeae Infection. Infectious Diseases and Therapy, 10(4), 1887–1905. https://doi.org/10.1007/s40121-021-00481-z
World Health Organization (2021). Guidelines for the management of symptomatic sexually transmitted infections. https://www.who.int/publications/i/item/9789240024168
Wynn, A., Bristow, C. C., Cristillo, A. D., Murphy, S. M., van den Broek, N., Muzny, C., Kallapur, S., Cohen, C., Ingalls, R. R., Wiesenfeld, H., Litch, J. A., Morris, S. R., & Klausner, J. D. (2020). Sexually Transmitted Infections in Pregnancy and Reproductive Health: Proceedings of the STAR Sexually Transmitted Infection Clinical Trial Group Programmatic Meeting. Sexually Transmitted Diseases, 47(1), 5–11. https://doi.org/10.1097/OLQ.0000000000001075
Zenebe, M. H., Mekonnen, Z., Loha, E., & Padalko, E. (2021). Prevalence, risk factors and association with delivery outcome of curable sexually transmitted infections among pregnant women in Southern Ethiopia. PLOS ONE, 16(3), e0248958. https://doi.org/10.1371/journal.pone.0248958
Copyright (c) 2023 Nadyah Haruna, Mochammad Hatta, Firdaus Hamid, Baedah Madjid, Muhammad Ilhamjaya, Monika Fitria Farid

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
Authors retain copyright and grant the journal right of first publication with the work simultaneously licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License that allows others to share the work with an acknowledgment of the work's authorship and initial publication in this journal.
Authors are able to enter into separate, additional contractual arrangements for the non-exclusive distribution of the journal's published version of the work (e.g., post it to an institutional repository or publish it in a book), with an acknowledgment of its initial publication in this journal.
Authors are permitted to publish their work online in third parties as it can lead to wider dissemination of the work.






