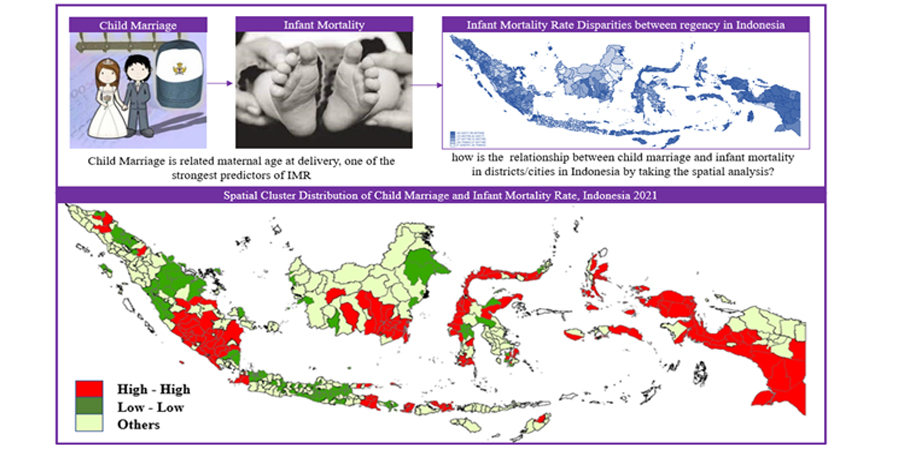
Child Marriage and Infant Mortality in Indonesia: A Spatial Analysis Approach
Abstract
Spatial analysis approach is capable of identifying spatial clustering of Infant Mortality Rate (IMR) across districts/cities in Indonesia. This information is essential for policymakers when developing appropriate health interventions at districts/cities level. At delivery, maternal age is one of the strongest predictors of infant mortality, which is closely related to child marriage. Therefore, this study aimed to determine the relationship between child marriage and IMR in Indonesia, which was controlled by the influence of maternal, household, and health factors. The results showed that there were spatial dependency on IMR in Indonesia. Analysis Regression Spatial Durbin Model showed that child marriage had a positive and significant relationship with IMR. Furthermore, it was discovered that IMR was influenced by several explanatory variables in districts and neighboring cities. To reduce mortality rate, there was a need to increase health services by developing neighboring areas and building access to areas with good health facilities. Educational initiatives are also important, emphasizing the importance of delaying the age of marriage and enforcing the minimum age limits. This approach empowered every child to marriage carefully and had good reproductive health knowledge that could decrease IMR in Indonesia.
Downloads
References
AIPI. (2013). Reducing maternal and neonatal mortality in Indonesia: Saving lives, saving the future. In Reducing Maternal and Neonatal Mortality in Indonesia: Saving Lives, Saving the Future. https://doi.org/10.17226/18437
Akaike, H. (1974) A New Look at the Model Selection Identification. IEEE Transactions on Automatic Control, 19, 716-723. http://dx.doi.org/10.1109/TAC.1974.1100705
Alam, M. B., Acharjee, S., Mahmud, S. M. A., Tania, J. A., Ali Khan, M. M., Islam, M. S., & Khan, M. N. (2022). Household air pollution from cooking fuels and its association with under-five mortality in Bangladesh. Clinical Epidemiology and Global Health, 17(May), 101134. https://doi.org/10.1016/j.cegh.2022.101134
Anselin, L., & Rey, S. J. (2014). Spatial Weights: Contiguity. Modern Spatial Econometrics in Practice: A Guide to GeoDa, GeoDaSpace and PySAL, 43.
Barufi, A. M., Haddad, E., & Paez, A. (2012). Infant mortality in Brazil, 1980-2000: A spatial panel data analysis. BMC Public Health, 12(1). https://doi.org/10.1186/1471-2458-12-181
BPS, BAPPENAS, UNICEF, & PUSKAPA. (2020). Prevention of Child Marriage: Acceleration that Cannot Wait. https://www.unicef.org/indonesia/sites/unicef.org.indonesia/files/2020-06/Prevention-of-Child-Marriage-Report-2020.pdf
Das, U., Chaplot, B., & Azamathulla, H. M. (2021). The Role of Place of Delivery in Preventing Neonatal and Infant Mortality Rate in India. Geographies, 1(1), 47–62. https://doi.org/10.3390/geographies1010004
Ertem, M., & Kocturk, T. (2008). Opinions on early-age marriage and marriage customs among Kurdish-speaking women in southeast Turkey. Journal of Family Planning and Reproductive Health Care, 34(3), 147–152. https://doi.org/10.1783/147118908784734927
Ertem, M., Saka, G., Ceylan, A., Deǧer, V., & Çiftçi, S. (2008). The factors associated with adolescent marriages and outcomes of adolescent pregnancies in Mardin Turkey. Journal of Comparative Family Studies, 39(2). https://doi.org/10.3138/jcfs.39.2.229
Garcia-Hombrados, J. (2021). Child marriage and infant mortality: causal evidence from Ethiopia. Journal of Population Economics, 1–61. https://doi.org/10.1007/s00148-021-00873-y
Gouda, J., Gupta, A. K., & Yadav, A. K. (2015). Association of child health and household amenities in high focus states in India: A district-level analysis. BMJ Open, 5(5), 1–11. https://doi.org/10.1136/bmjopen-2015-007589
Gupta, A. K., Ladusingh, L., & Borkotoky, K. (2016). Spatial clustering and risk factors of infant mortality: District-level assessment of highfocus states in India. Genus, 72(1). https://doi.org/10.1186/s41118-016-0008-9
Hathi, P., Haque, S., Pant, L., Coffey, D., & Spears, D. (2017). Place and Child Health: The Interaction of Population Density and Sanitation in Developing Countries. Demography, 54(1), 337–360. https://doi.org/10.1007/s13524-016-0538-y
Hossain, M. M., Abdulla, F., Banik, R., Yeasmin, S., & Rahman, A. (2022). Child marriage and its association with morbidity and mortality of under-5 years old children in Bangladesh. PLOS ONE, 17(2), 1–14. https://doi.org/10.1371/journal.pone.0262927
Jensen, R., & Thornton, R. (2003). Early female marriage in the developing world. Gender & Development, 11(2), 9–19. https://doi.org/10.1080/741954311
Kalipeni, E. (1993). Determinants of infant mortality in Malawi: A spatial perspective. Social Science and Medicine, 37(2), 183–198. https://doi.org/10.1016/0277-9536(93)90454-C
Ladusingh, L., & Singh, C. H. (2006). Place, community education, gender and child mortality in North-East India. Population, Space and Place, 12(1), 65–76. https://doi.org/10.1002/psp.393
Lawn, J. E., Cousens, S., & Zupan, J. (2005). 4 million neonatal deaths: When? Where? Why? Lancet, 365(9462), 891–900. https://doi.org/10.1016/S0140-6736(05)71048-5
LeSage, J. P. (1999). The Theory and Practice of Econometrics. University of Toledo. Toledo, Ohio. https://doi.org/10.2307/2553707
LeSage, J., & Pace, K. (2009). Introduction to spatial econometrics. (N. Balakrishnan & W. R. Schucany, Eds.). Texas: CRC press.
Levine, R. A., & Rowe, M. L. (2009). Maternal literacy and child health in less-developed countries: evidence, processes, and limitations. Journal of Developmental and Behavioral Pediatrics, 30(4), 340–349. http://www.doi.org/10.1097/DBP.0b013e3181b0eeff
Manda, S.O.M. (1999). Birth Intervals, Breastfeeding and Determinants of Childhood Mortality in Malawi. Social Science and Medicine 48:301-12. https://doi.org/10.1016/S0277-9536(98)00359-1
Mosley, W. H., & Chen, L. C. (1984). An Analytical Framework for the Study of Child Survival in Developing Countries. Population and Development Review, 10, 25–45. https://www.jstor.org/stable/2807954
Neal, S., Channon, A. A., & Chintsanya, J. (2018). The impact of young maternal age at birth on neonatal mortality: Evidence from 45 low and middle income countries. PLoS ONE, 13(5). https://doi.org/10.1371/journal.pone.0195731
Ozalp, S., Tanir, H. M., Sener, T., Yazan, S., & Keskin, A. E. (2003). Health risks for early (≤19) and late (≥35) childbearing. Archives of Gynecology and Obstetrics, 268(3), 172–174. https://doi.org/10.1007/s00404-002-0359-7
Poerwanto, S., Stevenson, M., & Klerk, N. De. (2003). Infant mortality and family welfare : policy implications for Indonesia. Journal of Epidemiology and Community Health, 57(7), 493–498. https://doi.org/10.1136%2Fjech.57.7.493
Pramono, M. S., Aditie, B., & Sutikno. (2012). Regresi spatial durbin model untuk mengidentifikasi faktor yang berpengaruh pada angka kematian bayi di Jawa Timur. Buletin Penelitian Kesehatan, 40(4), 190–200. https://dx.doi.org/10.22435/bpk.v40i4%20Des.2901.190-200
Raj, A., & Boehmer, U. (2013). Girl Child Marriage and Its Association With National Rates of HIV, Maternal Health, and Infant Mortality Across 97 Countries. Violence Against Women, 19(4), 536–551. https://doi.org/10.1177/1077801213487747
Raj, A., Saggurti, N., Winter, M., Labonte, A., Decker, M. R., Balaiah, D., & Silverman, J. G. (2010). The effect of maternal child marriage on morbidity and mortality of children under 5 in India: Cross sectional study of a nationally representative sample. BMJ, 340(b4258), 1–9. https://doi.org/10.1136/bmj.b4258
Ram, S. S., Ram, B., & Yadav, A. (2021). The Effects of Maternal Age on Neonatal and Post-neonatal Mortality in India: Roles of Socioeconomic and Biodemographic Factors. Canadian Studies in Population, 48, 59–89. https://doi.org/10.1007/s42650-021-00041-3
Rashid, M., & Chand, S. (2016). Spatial Analysis and Modeling of Infant Mortality Rate Using Conditional Autoregressive Model-A Case Study of Punjab, Pakistan. Pakistan Journal of Medical Research, 55(3), 75–83.
Rosenzweig, M. R., & Schultz, T. P. (1983). Estimating a Household Production Function : Heterogeneity , the Demand for Health Inputs , and Their Effects on Birth Weight. The University of Chicago Press Journals, 91(5), 723–746. https://www.jstor.org/stable/1837367
Santiago, R. D., & Tubayan, E. J. c. (2016). The Relationship of Health-Related Factors to Labor Productivity of the ASEAN-5. Review of Integrative Business and Economics Research, 5(4), 138–170. http://buscompress.com/journal-home.html
Santy, T. J. (2018). Pengaruh Ketimpangan Pendapatan Dan Kemiskinan Terhadap Tingkat Kematian Bayi Di Indonesia: Dalam Perspektif Spasial. Tesis. Universitas Indonesia.
Singh, A., Pathak, P. K., Chauhan, R. K., & Pan, W. (2011). Infant and child mortality in India in the last two decades: A geospatial analysis. PLoS ONE, 6(11). https://doi.org/10.1371/journal.pone.0026856
Solanke, B. L. (2015). Marriage Age, Fertility Behavior, and Women's Empowerment in Nigeria. SAGE Open, 5(4), 1–9. https://doi.org/10.1177/2158244015617989
Trommlerová, S. K. (2020). When children have children: The effects of child marriages and teenage pregnancies on early childhood mortality in Bangladesh. Economics and Human Biology, 39. https://doi.org/10.1016/j.ehb.2020.100904
Unicef (2023). Infant mortality rate. https://data.unicef.org/country/idn/
Weldearegawi, B., Melaku, Y. A., Abera, S. F., Ashebir, Y., Haile, F., Mulugeta, A., Eshetu, F., & Spigt, M. (2015). Infant mortality and causes of infant deaths in rural Ethiopia: A population-based cohort of 3684 births. BMC Public Health, 15(1). https://doi.org/10.1186/s12889-015-2090-x
WHO (2023). Newborn and Child Mortality: By 2030, End Preventable Deaths of Newborns and Children under 5 Years of Age, with All Countries Aiming to Reduce Neonatal Mortality and under-5 Mortality. https://www.who.int/data/gho/data/themes/topics/indicator-groups/indicator-group-details/GHO/sdg-target-3.2-newborn-and-child-mortality
Copyright (c) 2023 Nugrahayu Suryaningrum, Omas Bulan Samosir, Triasih Djutaharta

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
Authors retain copyright and grant the journal right of first publication with the work simultaneously licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License that allows others to share the work with an acknowledgment of the work's authorship and initial publication in this journal.
Authors are able to enter into separate, additional contractual arrangements for the non-exclusive distribution of the journal's published version of the work (e.g., post it to an institutional repository or publish it in a book), with an acknowledgment of its initial publication in this journal.
Authors are permitted to publish their work online in third parties as it can lead to wider dissemination of the work.