Parental Engagement in Promoting Awareness of Contraceptive Use among Female Students in Nigeria and Cameroon
Abstract
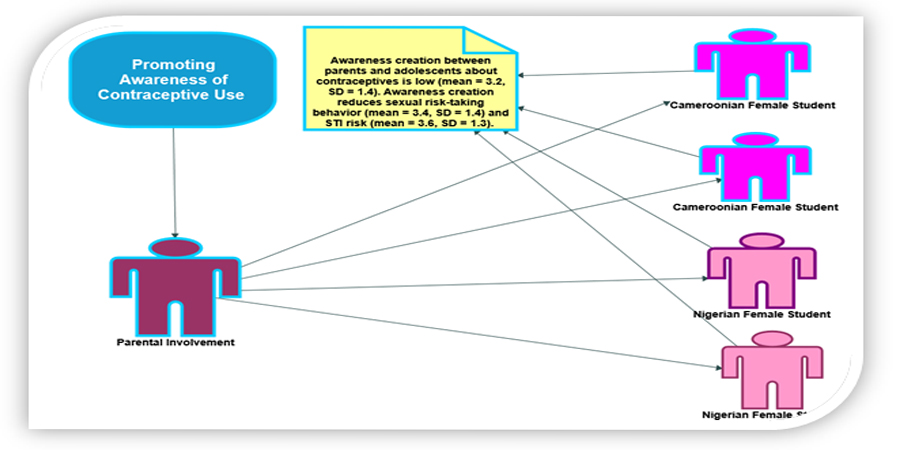
Despite government and non-governmental organizations' efforts, contraceptive utilization in Nigeria remains low. Similarly, Cameroon faces high maternal mortality and low contraceptive prevalence. Adolescent pregnancy remains a significant social and public health concern globally, necessitating efforts to promote contraceptive use. Parent-adolescent sexual communication is often viewed as taboo in Nigeria and Cameroon, hindering awareness about contraceptive use. This study examines the role of parents in creating awareness of contraceptive use among female university students in Nigeria and Cameroon. The study adopts a comparative approach, investigating the cultural role of parents in awareness creation for contraceptive use in Nigeria and Cameroon. A cross-sectional study was conducted among 420 female university students in both countries. The findings highlight the valuable role of parents in shaping adolescents' knowledge and behavior regarding contraceptive use. Recommendations include enhancing comprehensive sexual and reproductive health education, promoting parent-adolescent communication, addressing cultural barriers, improving contraceptive access, and conducting further research. Implementing these recommendations can empower adolescents with accurate information, foster supportive parent-adolescent relationships, and enhance sexual and reproductive health outcomes among young people.
Downloads
References
Abdallah, A. K., Magata, R. J., & Sylvester J. N. (2017). Barriers to parent-child communication on sexual and reproductive health issues in East Africa: A review of qualitative research in four countries. J African Stud Dev. 9:45–50. https://doi.org/10.5897/JASD2016.0410
Akinyemi, O. O., Harris, B., & Kawonga, M. (2020). ‘Our culture prohibits some things’: qualitative inquiry into how sociocultural context influences the scale-up of community-based injectable contraceptives in Nigeria. BMJ open, 10(7), e035311. https://doi.org/10.1136/bmjopen-2019-035311
Akoku, D. A., Vukugah, T. A., Tihnje, M. A., & Nzubepie, I. B. (2020). Oral contraceptive use and premenstrual syndrome among sexually active female university students in Cameroon. Pan African Medical Journal, 36(1). http://www.doi.org/10.11604/pamj.2020.36.333.25078
Ali, A. (2015). " I Got Peace and Stability": Women's Perceptions of Contraceptive Use in Sidama, SNNPR, Ethiopia (Doctoral dissertation, University of Saskatchewan). https://harvest.usask.ca/items/6c2aa4c2-9e0c-418f-b71e-1d627f1bb70e
Ariyo, A. M., Sotayo, O. M., Olurin, T. K., & Eni-Olorunda, T. (2020). Sexual Communication between Parents and Adolescents: Perception of Secondary School Students in Abeokuta, Ogun State, Nigeria. Mediterranean Journal of Social Sciences, 11(4), 112. https://doi.org/10.36941/mjss-2020-004
Atuhaire, S., Ngendakumana, J., Galadima, A., Adam, A., & Muderhwa, R. B. (2021). Knowledge and attitude towards contraceptive use among adolescents in Africa: a systematic review. Int J Reprod Contraception Obstet Gynecol, 10(11), 4292-303. https://dx.doi.org/10.18203/2320-1770.ijrcog2021434
Bekele, D., Deksisa, A., Abera, W., & Megersa, G. (2022). Parental communication on sexual and reproductive health issues to their adolescents and affecting factors at Asella town, Ethiopia: a community-based, cross-sectional study. Reproductive Health, 19(1), 114. https://doi.org/10.1186/s12978-022-01408-8
Blackstone, S. R., Nwaozuru, U., Iwelunmor, J. (2017). Factors Influencing Contraceptive Use in Sub-Saharan Africa: A Systematic Review. Int Q Community Health Educ. 37(2):79-91. https://doi.org/10.1177/0272684X16685254
Bradley, P. S., Carling, C., Diaz, A. G., Hood, P., Barnes, C., Ade, J., & Mohr, M. (2013). Match performance and physical capacity of players in the top three competitive standards of English professional soccer. Human movement science, 32(4), 808-821. https://doi.org/10.1016/j.humov.2013.06.002
Dombola, G. M., Manda, W. C., & Chipeta, E. (2021). Factors influencing contraceptive decision making and use among young adolescents in urban Lilongwe, Malawi: a qualitative study. Reproductive Health, 18, 1-11. http://www.doi.org/10.1186/s12978-021-01259-9
Esan, D. T., & Bayajidda, K. K. (2021). The perception of parents of high school students about adolescent sexual and reproductive needs in Nigeria: A qualitative study. Public Health in Practice, 2, 100080. https://doi.org/10.1016/j.puhip.2021.100080
Eshete, A., & Shewasinad, S. (2020). Adolescent-parent communication on sexual and reproductive health issues in Ethiopia: a systematic review and meta-analysis. Ethiopian Journal of Health Sciences, 30(5). https://doi.org/10.4314/ejhs.v30i5.22
Evans, R., Widman, L., Kamke, K., & Stewart, J. L. (2020). Gender differences in parents’ communication with their adolescent children about sexual risk and sex-positive topics. The Journal of Sex Research, 57(2), 177-188. https://doi.org/10.1080/00224499.2019.1661345
Ezenwaka, U., Mbachu, C., Ezumah, N., Eze, I., Agu, C., Agu, I., & Onwujekwe, O. (2020). Exploring factors constraining utilization of contraceptive services among adolescents in Southeast Nigeria: an application of the socio-ecological model. BMC Public Health, 20, 1-11. https://doi.org/10.1186/s12889-020-09276-2
Fanta, M., Lemma, S., Gamo, G., & Meskele, M. (2016). Factors associated with adolescent parent communication of reproductive health issues among high school and preparatory students in Boditi town, Southern Ethiopia: a cross-sectional study, Patient Intelligence, vol. 8, pp. 57–70, 2016. https://doi.org/10.2147/PI.S97838
Forehand, R., Lafko, N., Parent, J., & Burt, K. B. (2014). Is parenting the mediator of change in behavioral parent training for externalizing problems of youth?. Clinical psychology review, 34(8), 608-619. https://doi.org/10.1016/j.cpr.2014.10.001
Jiménez-Iglesias, A. Moreno, C. García-Moya, I.& Rivera, F. (2018). Prevalence of emergency contraceptive pill use among Spanish adolescent girls and their family and psychological profiles. BMC Women’s Health, 18, 1-8. https://doi.org/10.1186/s12905-018-0560-x
Kara, W. S. K., Benedicto, M., & Mao, J. (2019). Knowledge, attitude, and practice of contraception methods among female undergraduates in Dodoma, Tanzania. Cureus, 11(4). http://www.doi.org/10.7759/cureus.4362
Kassa, G. M., Arowojolu, A. O., Odukogbe, A. A., & Yalew, A. W. (2018). Prevalence and determinants of adolescent pregnancy in Africa: a systematic review and meta-analysis. Reproductive health, 15(1), 1-17. https://doi.org/10.1186/s12978-018-0640-
KWASU (2020). Administrative Unit, Kwara State University, Malete, Nigeria.
Morales, A. Orgilés, M. & Espada, J.P. (2020). Sexually Unexperienced Adolescents Benefit the Most From a Sexual Education Program for Adolescents: A Longitudinal Cluster Randomized Controlled Study. AIDS Educ. Prev. 32, 493–511. https://doi.org/10.1521/aeap.2020.32.6.493
Neil, C. & Donald. (2015). Important life issues. European Scientific Journal, 11(20), 1857-7881.
Okonofua, F. (2021). Maternal Mortality in Developing Countries. Contemporary Obstetrics and Gynecology for Developing Countries, 13-22. https://doi.org/10.1007/978-3-030-75385-6_3
Ononokpono, D. N., Odimegwu, C. O., & Usoro, N. A. (2020). Contraceptive use in Nigeria: does social context matter?. African Journal of Reproductive Health, 24(1), 133-142. http://www.doi.org/10.29063/ajrh2020/v24i1.14
Patton, G. C., Sawyer, S. M., Santelli, J. S., Ross, D. A., Afifi, R., Allen, N. B., & Viner, R. M. (2016). Our future: a Lancet commission on adolescent health and wellbeing. The Lancet, 387(10036), 2423-2478. https://doi.org/10.1016/s0140-6736(16)00579-
Sagnia, P. I., Gharoro, E. P., & Isara, A. R. (2020). Adolescent-parent communication on sexual and reproductive health issues amongst secondary school students in Western Region 1 of The Gambia. African Journal of Primary Health Care and Family Medicine, 12(1), 1-7. https://hdl.handle.net/10520/ejc-phcfm-v12-n1-a87
Sinai, I., Omoluabi, E., Jimoh, A., & Jurczynska, K. (2020). Unmet need for family planning and barriers to contraceptive use in Kaduna, Nigeria: culture, myths and perceptions. Culture, health & sexuality, 22(11), 1253-1268. https://doi.org/10.1080/13691058.2019.1672894
Sedgh, G., Finer, L. B., Bankole, A., Eilers, M. A., & Singh, S. (2015). Adolescent pregnancy, birth, and abortion rates across countries: levels and recent trends. Journal of adolescent health, 56(2), 223-230. https://doi.org/10.1016/j.jadohealth.2014.09.007
Tchokossa, M. A., & Adeyemi, B. A. (2018). Knowledge and use of contraceptives among female adolescents in selected senior secondary schools in Ife central local government of Osun state. J Commu Med Health Edu. 08(03):1647-61.
Tebeu, P. M., Halle-Ekane, G., Da Itambi, M., Mbu, R. E., Mawamba, Y., & Fomulu, J. N. (2015). Maternal mortality in Cameroon: a university teaching hospital report. Pan African Medical Journal, 21(1). https://doi.org/10.11604/pamj.2015.22.377.8631
Ugoji, F.N. & Agokei, R.C. (2012). Rural Nursing Students’ Knowledge of HIV/AIDS, and Beliefs and their Attitude Towards People Living with HIV/AIDS. International Journal of Psychology and Behavioral Sciences,2(6): 226-230. http://www.doi.org/10.5923/j.ijpbs.20120206.05.
Unilorin (2020). Academic Planning Office, Main Campus, University of Ilorin, Nigeria
Wang, Y., Chen, M., Tan, S., Qu, X., Wang, H., Liang, X., & Tang, K. (2020). The socioeconomic and lifestyle determinants of contraceptive use among Chinese college students: a cross-sectional study. Reproductive Health, 17, 1-11. https://doi.org/10.1186/s12978-020-00978-9
World Health Organization. (2018). WHO recommendations on adolescent sexual and reproductive health and rights. https://iris.who.int/bitstream/handle/10665/275374/9789241514606-eng.pdf
World Health Organization (2023). Maternal mortality: The urgency of a systemic and multisectoral approach in mitigating maternal deaths in Africa.. https://files.aho.afro.who.int/afahobckpcontainer/production/files/iAHO_Maternal_Mortality_Regional_Factsheet.pdf
Widman, L., Choukas-Bradley, S., Noar, S. M., Nesi, J., & Garrett, K. (2016). Parent-adolescent sexual communication and adolescent safer sex behavior: A meta-analysis. JAMA pediatrics, 170(1), 52-61. http://www.doi.org/10.1001/jamapediatrics.2015.2731
Zhou, Y., Wang, T., Fu, J., Chen, M., Meng, Y., & Luo, Y. (2019). Access to reproductive health services among the female floating population of childbearing age: a cross-sectional study in Changsha, China. BMC Health Services Research, 19, 1-10. https://doi.org/10.1186/s12913-019-4334-4
Copyright (c) 2023 Rasaq Muhammed Adisa, Fabiolla Michelle Masso, Patrick Udende, Yusuf Ajani Sholola, Mahamood Ahmad Fahmi, Oba Abdulkadir La'aro

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
Authors retain copyright and grant the journal right of first publication with the work simultaneously licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License that allows others to share the work with an acknowledgment of the work's authorship and initial publication in this journal.
Authors are able to enter into separate, additional contractual arrangements for the non-exclusive distribution of the journal's published version of the work (e.g., post it to an institutional repository or publish it in a book), with an acknowledgment of its initial publication in this journal.
Authors are permitted to publish their work online in third parties as it can lead to wider dissemination of the work.






