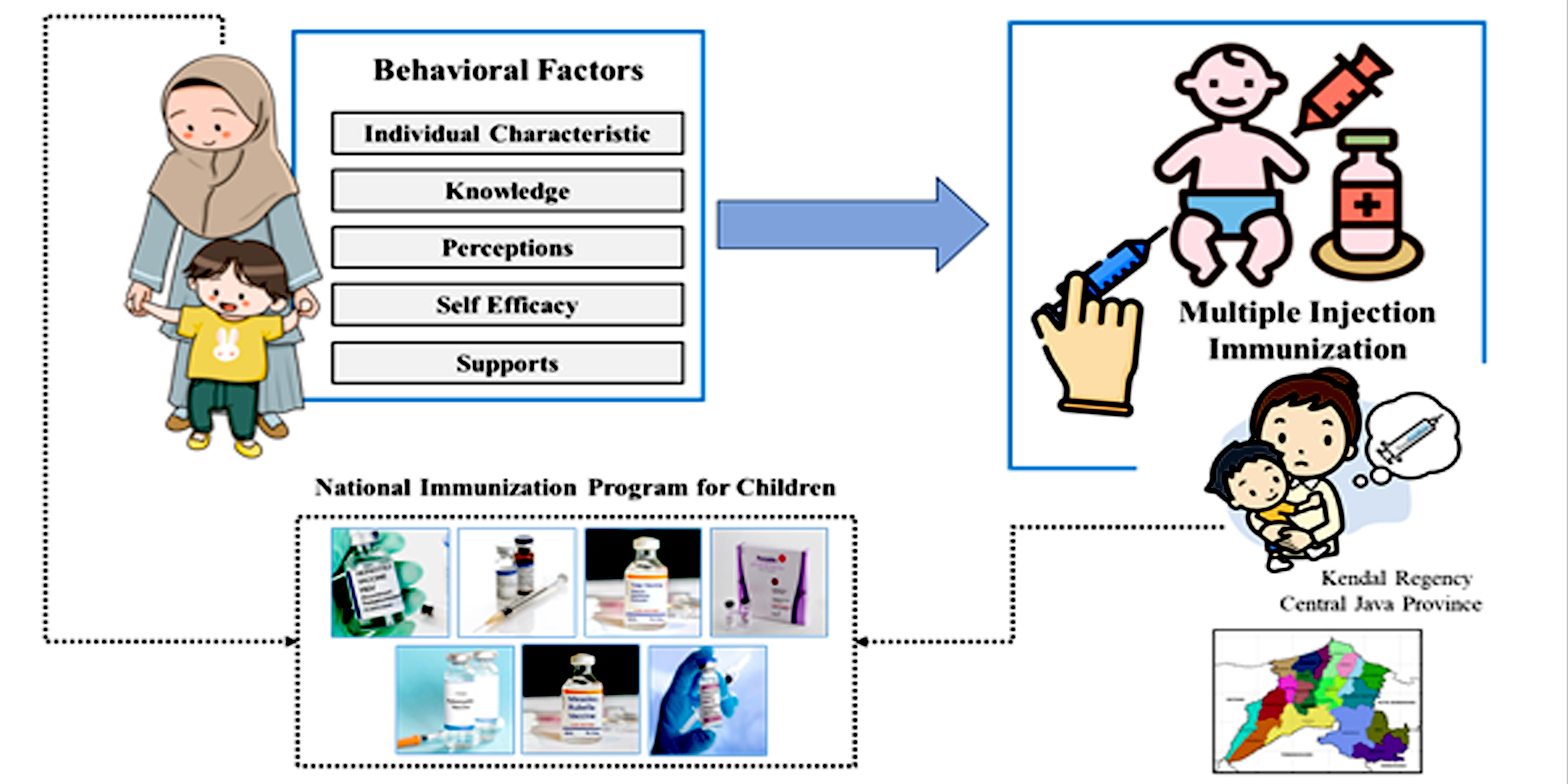
Behavioral Factors and Practices of Multiple Injection Immunization for Children Aged 9-12 Months in Rural Areas
Abstract
Immunization has been proven to be cost-effective and globally successful in reducing child deaths from infectious diseases. However, the many types of vaccines that must be given to each child in one visit make this practice controversial because they are considered unsafe. The study aims to analyze behavioral determinants of multiple injection immunization practices in rural areas. This is analytical research with a quantitative and cross-sectional approach. The population consists of all children aged 9-12 months in Kendal Regency with a sample of 407 children. Respondents were parents/caregivers selected from 30 PHC. Data were collected by interview using a questionnaire that had been tested for validity and reliability. Immunization practices are assessed through the Maternal and Child Health-Book. Immunization practice with multiple injections is partially related to education, knowledge, perception (susceptibility, severity, side effects, benefits), self-efficacy, and support (family, health workers, community, informational, and policy). Simultaneously, it is known that health worker support has the most dominant influence, followed by informational support, knowledge, perceived severity, and perceived susceptibility. Efforts are needed to increase health workers' competency in reducing the pain of children due to vaccination, as well as providing education to parents/caregivers effectively through clear communication, reducing misinformation and misperceptions, especially for rural communities.
Downloads
References
Abukhaled, M., & Cortez, S. (2021). Nonpharmacological Methods for Reducing Parental Concern for Infant Vaccine-Associated Pain. Journal of Pediatric Health Care, 35(2), 180–187. https://doi.org/10.1016/j.pedhc.2020.09.006
Agrawal, A., Kolhapure, S., Di Pasquale, A., Rai, J., & Mathur, A. (2020). Vaccine Hesitancy as a Challenge or Vaccine Confidence as an Opportunity for Childhood Immunisation in India. Infectious Diseases and Therapy, 9(3), 421–432. https://doi.org/10.1007/s40121-020-00302-9
Albers, A. N., Thaker, J., & Newcomer, S. R. (2022). Barriers to and facilitators of early childhood immunization in rural areas of the United States: A systematic review of the literature. Preventive Medicine Reports, 27(April), 101804. https://doi.org/10.1016/j.pmedr.2022.101804
Alghofaili, M. A., Aljuaid, S. O., Alqahtani, N., Alghufaili, M., & Abd-Ellatif, E. E. (2023). Factors Contributing to the Delayed Vaccination Among Children in Riyadh City, Saudi Arabia: A Cross-Sectional Study. Cureus, 15(Mcv), 1–14. https://doi.org/10.7759/cureus.43188
Althumairi, A., Sahwan, M., Alsaleh, S., Abduljabbar, Z., & Aljabri, D. (2021). Virtual reality: Is it helping children cope with fear and pain during vaccination? Journal of Multidisciplinary Healthcare, 14, 2625–2632. https://doi.org/10.2147/JMDH.S327349
Ateudjieu, J., Yakum, M. N., Goura, A. P., Tembei, A. M., Ingrid, D. K., Bita’A Landry, B., Kenfack, B., Amada, L., Tadzong, I., & Bissek, A. C. (2020). EPI immunization coverage, timeliness and dropout rate among children in a West Cameroon health district: A cross sectional study. BMC Public Health, 20(1), 1–11. https://doi.org/10.1186/s12889-020-8340-6
Bausad, A. A. P., & Muchlisa, N. (2022). Faktor yang Mempengaruhi Cakupan dan Ketepatan Waktu Imunisasi. Jurnal Kesehatan Ilmiah Indonesia, 7(2), 161–166. https://jurnal.unar.ac.id/index.php/health/article/view/915/565
Bianco, A., Mascaro, V., Zucco, R., & Pavia, M. (2019). Parent perspectives on childhood vaccination: How to deal with vaccine hesitancy and refusal? Vaccine, 37(7), 984–990. https://doi.org/10.1016/j.vaccine.2018.12.062
Chu, H., & Rammohan, A. (2022). Childhood immunization and age-appropriate vaccinations in Indonesia. BMC Public Health, 22(1), 1–12. https://doi.org/10.1186/s12889-022-14408-x
Deschanvres, C., Levieux, K., Launay, E., Huby, A. C., Scherdel, P., de Visme, S., Hanf, M., & Gras-Le Guen, C. (2023). Non-immunization associated with increased risk of sudden unexpected death in infancy: A national case–control study. Vaccine, 41(2), 391–396. https://doi.org/10.1016/j.vaccine.2022.10.087
Destefano, F., Bodenstab, H. M., & Offit, P. A. (2019). Principal Controversies in Vaccine Safety in the United States. Clinical Infectious Diseases, 69(4), 726–731. https://doi.org/10.1093/cid/ciz135
Dirirsa, K., Makuria, M., Mulu, E., & Deriba, B. S. (2022). Assessment of vaccination timeliness and associated factors among children in Toke Kutaye district, central Ethiopia: A Mixed study. PLoS ONE, 17(1 January), 1–17. https://doi.org/10.1371/journal.pone.0262320
Dolan, S. B., Patel, M., Hampton, L. M., Burnett, E., Ehlman, D. C., Garon, J., Cloessner, E., Chmielewski, E., Hyde, T. B., Mantel, C., & Wallace, A. S. (2017). Administering Multiple Injectable Vaccines during a Single Visit - Summary of Findings from the Accelerated Introduction of Inactivated Polio Vaccine Globally. Journal of Infectious Diseases, 216(April (Suppl 1)), S152–S160. https://doi.org/10.1093/infdis/jix054
Dubé, È., Ward, J. K., Verger, P., & MacDonald, N. E. (2021). Vaccine Hesitancy , Acceptance , and Anti-Vaccination : Trends and Future Prospects for Public Health. Annual Review of Public Health, 42, 175–191. http://www.orspaca.org/sites/default/files/annurev-publhealth-vaccine-hesitancy.pdf
Facciola, A., Visalli, G., Orlando, A., Bertuccio, M. P., Spataro, P., Squeri, R., Picerno, I., & Di Pietro, A. (2019). Vaccine hesitancy: An overview on parents’ opinions about vaccination and possible reasons of vaccine refusal. Journal of Public Health Research, 8(1), 13–18. https://doi.org/10.4081/jphr.2019.1436
Finkelstein, S. R., Boland, W. A., Vallen, B., Connell, P. M., Sherman, G. D., & Feemster, K. A. (2020). Psychological reactance impacts ratings of pediatrician vaccine-related communication quality, perceived vaccine safety, and vaccination priority among U.S. parents. Human Vaccines and Immunotherapeutics, 16(5), 1024–1029. https://doi.org/10.1080/21645515.2019.1694815
Garcia, É. M., Souza, E. L. de, Matozinhos, F. P., Silva, T. M. R. da, Waldman, E. A., & Sato, A. P. S. (2023). Associated factors with vaccine hesitancy in mothers of children up to two years old in a Brazilian city. PLOS Global Public Health, 3(6), e0002026 (1-15). https://doi.org/10.1371/journal.pgph.0002026
Ghosh, A., Annigeri, S., Hemram, S. K., Dey, P. K., Mazumder, S., & Ghosh, P. (2022). Demography and determinants of incomplete immunization in children aged 1–5 years and vaccine-hesitancy among caregivers: An Eastern Indian perspective. Clinical Epidemiology and Global Health, 17, 101155.. https://doi.org/10.1016/j.cegh.2022.101155
Ghosh, A., & Laxminarayan, R. (2017). Demand-and supply-side determinants of diphtheria-pertussis-tetanus nonvaccination and dropout in rural India. Vaccine, 35(7), 1087-1093. https://doi.org/10.1016/j.vaccine.2016.12.024
Giannakou, K., Kyprianidou, M., Hadjikou, A., Fakonti, G., Photiou, G., Tzira, E., & Heraclides, A. (2021). Knowledge of mothers regarding children’s vaccinations in Greece: an online cross-sectional study. BMC Public Health, 21(1), 1–13. https://doi.org/10.1186/s12889-021-12179-5
Hasnan, S., & Tan, N. C. (2021). Multi-domain narrative review of vaccine hesitancy in childhood. Vaccine, 39(14), 1910–1920. https://doi.org/10.1016/j.vaccine.2021.02.057
Ijarotimi, I. T., Fatiregun, A. A., Adebiyi, O. A., Ilesanmi, O. S., & Ajumobi, O. (2018). Urban–rural differences in immunisation status and associated demographic factors among children 12-59 months in a Southwestern state, Nigeria. PLoS ONE, 13(11), 1–11. https://doi.org/10.1371/journal.pone.0206086
Kagoné, M., Yé, M., Nébié, E., Sié, A., Müller, O., & Beiersmann, C. (2018). Community perception regarding childhood vaccinations and its implications for effectiveness: a qualitative study in rural Burkina Faso. BMC Public Health, 18(324), 1–10. https://doi.org/https://doi.org/10.1186/s12889-018-5244-9
Kanchan, M. I., Firoz, M., Kurlikar, P. R., Chourase, M., Yadav, R., & Biswas, A. B. (2018). Status and determinants of child immunisation coverage in three South Asian countries, India, Bangladesh and Nepal: Evidence from the Demographic and Health Survey. Sri Lanka Journal of Child Health, 47(1), 56–63. https://doi.org/10.4038/sljch.v47i1.8431
Kassab, M., Hamadneh, S., Nuseir, K., ALmomani, B., & Hamadneh, J. (2018). Factors Associated With Infant Pain Severity Undergoing Immunization Injections. Journal of Pediatric Nursing, 42, e85–e90. https://doi.org/10.1016/j.pedn.2018.04.002
Ministry of Health RI. (2019). Laporan Nasional Riskesdas 2018. In Badan Penelitian dan Pengembangan, Kementerian Kesehatan RI (Vol. 1, Issue 1). https://www.kemkes.go.id/article/view/19093000001/penyakit-jantung-penyebab-kematian-terbanyak-ke-2-di-indonesia.html
Kiely, M., Boulianne, N., Talbot, D., Ouakki, M., Guay, M., Landry, M., Sauvageau, C., & De Serres, G. (2018). Impact of vaccine delays at the 2, 4, 6 and 12 month visits on incomplete vaccination status by 24 months of age in Quebec, Canada. BMC Public Health, 18(1), 1–15. https://doi.org/10.1186/s12889-018-6235-6
Moon, R. Y., Carlin, R. F., & Hand, I. (2022). Sleep-Related Infants Deaths: Updated 2022 Recommendations for Reducing Infant Deaths in the Sleep Environment. Pediatrics, 150(6), 1–22. https://doi.org/10.1542/peds.2022-059737Ahttps://doi.org/10.1542/peds.2022-057990
Nair, A. T., Nayar, K. R., Koya, S. F., Abraham, M., Lordson, J., Grace, C., Sreekumar, S., Chembon, P., Swarnam, K., Pillai, A. M., & Pandey, A. K. (2021). Social media, vaccine hesitancy and trust deficit in immunization programs: a qualitative enquiry in Malappuram District of Kerala, India. Health Research Policy and Systems, 19 (Supp 2(56), 1–8. https://doi.org/10.1186/s12961-021-00698-x
Nalley, J., & Maduka, O. (2019). Completeness and timeliness of immunization among children aged 12 to 23 months in South-South Nigeria. Journal of Community Medicine and Primary Health Care, 31(1), 22–31. https://doi.org/10.4314/JCMPHC.V31I1
Oktadevi, D., Sriatmi, A., & Kusumastuti, W. (2022). Karakteristik Ibu dalam Ketepatan Waktu Imunisasi Measles Rubella Selama Pandemi Covid-19 di Puskesmas Tempuran Kabupaten Magelang. Media Kesehatan Masyarakat Indonesia, 21(3), 148–152. https://doi.org/10.14710/mkmi.21.3.148-152
Panting, A. J., Zin, Z. M., Jaafar, N., Perialathan, K., Ilman, S. S. S., & Zakaria, M. R. (2018). Potential Factors Contributing to Vaccine Hesitancy among Parents in Malaysia: An Overview. International Journal of Health Sciences & Research (Www.Ijhsr.Org), 8(7), 360. www.ijhsr.org
Sapçi, E., Bilsin Kocamaz, E., & Gungormus, Z. (2021). Effects of applying external cold and vibration to children during vaccination on pain, fear and anxiety. Complementary Therapies in Medicine, 58(November 2020), 102688. https://doi.org/10.1016/j.ctim.2021.102688
Singh, S., Sahu, D., Agrawal, A., & Vashi, M. D. (2019). Barriers and opportunities for improving childhood immunization coverage in slums: A qualitative study. Preventive Medicine Reports, 14(March), 100858. https://doi.org/10.1016/j.pmedr.2019.100858
Siramaneerat, I., & Agushybana, F. (2021). Inequalities in immunization coverage in Indonesia: a multilevel analysis. Rural and Remote Health, 21(3), 1–11. https://doi.org/10.22605/rrh6348
Soveri, A., Karlsson, L. C., Mäki, O., Antfolk, J., Waris, O., Karlsson, H., Karlsson, L., Lindfelt, M., & Lewandowsky, S. (2020). Trait reactance and trust in doctors as predictors of vaccination behavior, vaccine attitudes, and use of complementary and alternative medicine in parents of young children. PLoS ONE, 15(7 July), 1–16. https://doi.org/10.1371/journal.pone.0236527
Sriatmi, A., Martini, M., Agushybana, F., Jati, S. P., Astorina, N., Handayani, N., & Nandini, N. (2021). Complete Basic Immunization Coverage among Infants in Temanggung Regency. Jurnal Aisyah: Jurnal Ilmu Kesehatan, 6(4), 645–650. https://doi.org/10.30604/jika.v6i4.815
Subramonian, A., & Featherstone, R. (2020). Interventions for the Prevention of Sudden Infant Death Syndrome and Sudden Unexplained Death in Infancy: a Review of Guidelines. CADTH; Rapid Response Service, 1(September 14), 1–24. https://www.ncbi.nlm.nih.gov/books/NBK566620/
UNICEF. (2023). For Every Child: Vaccination (Regional Brief). In East Asia and The Pacific-The State of The World’s Children 2023 (pp. 0–23). https://www.unicef.org/media/138981/file/Estado%20Mundial%20de%20la%20Infancia%202023.pdf
Viggiano, C., Occhinegro, A., Siano, M. A., Mandato, C., Adinolfi, M., Nardacci, A., Caiazzo, A. L., Viggiano, D., & Vajro, P. (2021). Analgesic effects of breast- and formula feeding during routine childhood immunizations up to 1 year of age. Pediatric Research, 89(5), 1179–1184. https://doi.org/10.1038/s41390-020-0939-x
Wang, P., Fan, W., & Li, Q. (2020). The alleviation effect of knowledge integration on anxiety in parental vaccine decision-making supported by online communities. Journal of Knowledge Management, 25(6), 1575–1593. https://doi.org/10.1108/JKM-05-2020-0329
World Health Organization. (2021). Module 8: Safety and acceptability of multiple injections. In Training for Inactivated Poliovirus Vaccine (IPV) Introduction (pp. 1–20). https://cdn.who.int/media/docs/default-source/immunization/multiple-injections/training_mod8_multiple_injections-june2016.pdf
World Health Organization. (2023). Immunization Coverage: Fact Sheet. World Health Organization. https://www.who.int/news-room/fact-sheets/detail/immunization-coverage
Yang, Y. T., & Shaw, J. (2018). Sudden infant death syndrome, attention-deficit/hyperactivity disorder and vaccines: Longitudinal population analyses. Vaccine, 36(5), 595–598. https://doi.org/10.1016/j.vaccine.2017.12.065
Copyright (c) 2024 Ayun Sriatmi, Setyo Endah Pratiwi , Farid Agushybana

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
Authors retain copyright and grant the journal right of first publication with the work simultaneously licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License that allows others to share the work with an acknowledgment of the work's authorship and initial publication in this journal.
Authors are able to enter into separate, additional contractual arrangements for the non-exclusive distribution of the journal's published version of the work (e.g., post it to an institutional repository or publish it in a book), with an acknowledgment of its initial publication in this journal.
Authors are permitted to publish their work online in third parties as it can lead to wider dissemination of the work.






