Preconception Health of Prospective Brides and Grooms in Malang Regency, Indonesia
Abstract
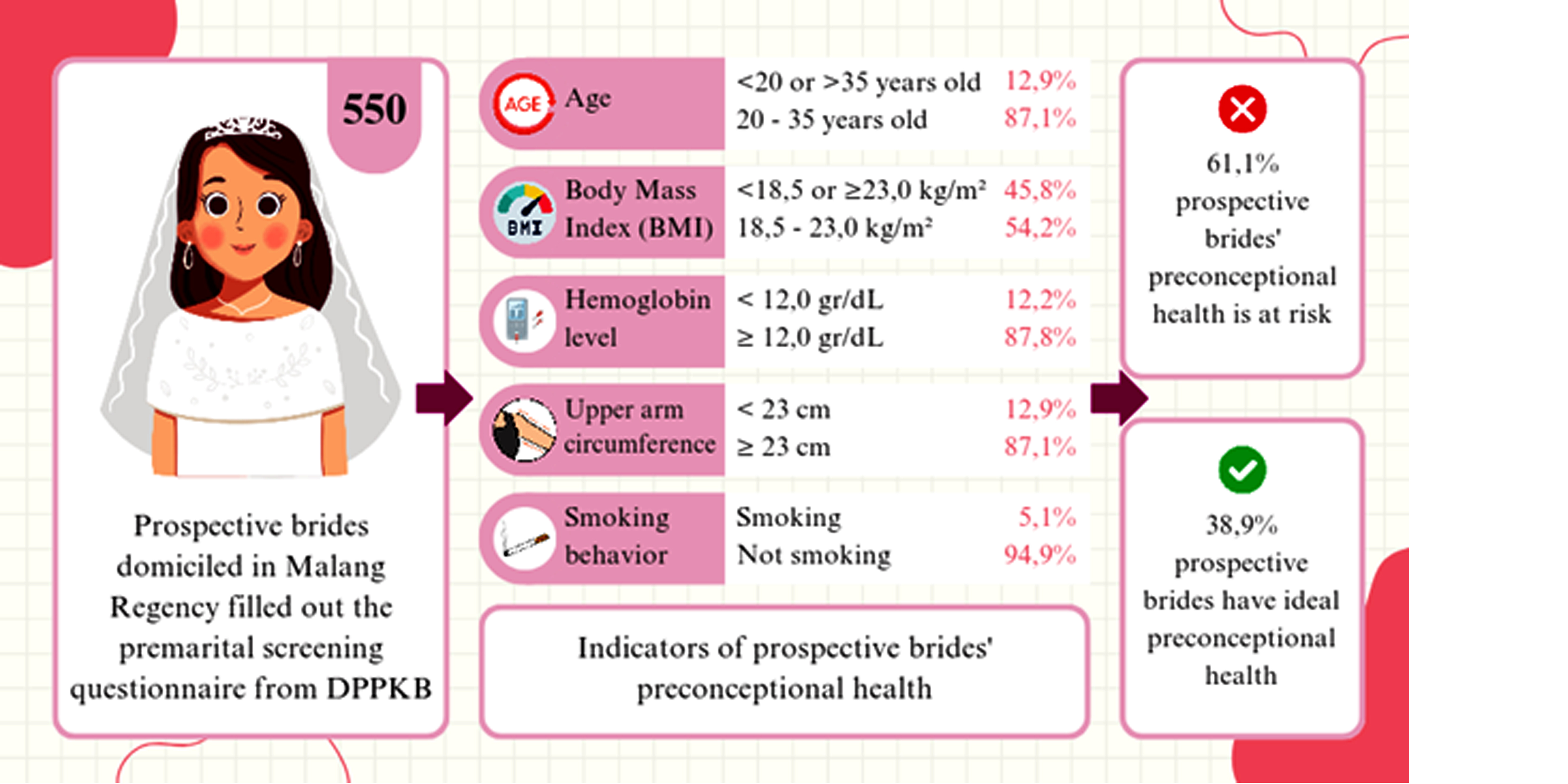
Preconception health is a significant contributor to pregnancy outcomes. However, the majority of women only improve their health status after receiving counseling at the first antenatal visit or during pregnancy. This shows the need to identify preconception health through premarital screening. Therefore, this study aimed to assess the characteristics of preconception health of prospective brides in Malang Regency using "Elsimil Application". The assessment was carried out using a quantitative descriptive method with a secondary data analysis. The total sampling method was used for sample collection and data used were obtained from prospective brides who completed the premarital screening questionnaire on Elsimil Application. The variables assessed were prospective brides’ preconception health with several sub-variables. These included age, BMI, Hb levels, upper arm circumference, and smoking behavior, which were collected using an instrument in the form of a checklist table. The results of the descriptive statistical analysis, which included the frequency and percentage, showed that a significant proportion of prospective brides had preconception health state at risk (61.1%). Consequently, this study recommended the importance of strengthening preconception health services by providing education, which comprised accurate information, accessibility, and required improvement, particularly for prospective brides and grooms in rural areas.
Downloads
References
Abbas, F., Kumar, R., Mahmood, T., & Somrongthong, R. (2021). Impact of children born with low birth weight on stunting and wasting in Sindh province of Pakistan: a propensity score matching approach. Scientific Reports, 11(1), 1–10. https://doi.org/10.1038/s41598-021-98924-7
Abuaisha, M., Itani, H., El Masri, R., & Antoun, J. (2020). Prevalence of iron deficiency (ID) without anemia in the general population presenting to primary care clinics: a cross-sectional study. Postgraduate medicine, 132(3), 282-287. https://doi.org/10.1080/00325481.2020.1715701
Amaje, E., Fikrie, A., & Utura, T. (2022). Utilization of Preconception Care and Its Associated Factors among Pregnant Women of West Guji Zone, Oromia, Ethiopia, 2021: A Community-Based Cross-Sectional Study. Health Services Research and Managerial Epidemiology, 9, 1–10. https://doi.org/10.1177/23333928221088720
Avşar, T. S., McLeod, H., & Jackson, L. (2021). Health outcomes of smoking during pregnancy and the postpartum period: an umbrella review. BMC Pregnancy and Childbirth, 21(254), 1–9. https://doi.org/10.1186/s12884-021-03729-1
Barker, M., Dombrowski, S. U., Colbourn, T., Fall, C. H., Kriznik, N. M., Lawrence, W. T., & Stephenson, J. (2018). Intervention strategies to improve nutrition and health behaviours before conception. The Lancet, 391(10132), 1853-1864. https://doi.org/10.1016/S0140-6736(18)30313-1
Basrowi, R. W., & Dilantika, C. (2021). Optimizing iron adequacy and absorption to prevent iron deficiency anemia: the role of combination of fortified iron and vitamin C. World Nutrition Journal, 5(S1), 33-39. https://doi.org/10.25220/WNJ.V05.S1.0005
Benowitz, N. L., & Liakoni, E. (2022). Tobacco use disorder and cardiovascular health. Addiction, 117(4), 1128-1138. https://doi.org/10.1111/add.15703
Boutari, C., Pappas, P. D., Mintziori, G., Nigdelis, M. P., Athanasiadis, L., Goulis, D. G., & Mantzoros, C. S. (2020). The effect of underweight on female and male reproduction. Metabolism Clinical and Experimental, 107(1), 1–14. https://doi.org/10.1016/j.metabol.2020.154229
Centers for Disease Control and Prevention. (2017). Youth risk behavior survey: Data summary & trends report. https://www.cdc.gov/healthyyouth/data/yrbs/yrbs_data_summary_and_trends.htm
D’Souza, R., Horyn, I., Pavalagantharajah, S., Zaffar, N., & Jacob, C. E. (2019). Maternal body mass index and pregnancy outcomes: a systematic review and metaanalysis. American Journal of Obstetrics and Gynecology MFM, 1(4), 100041. https://doi.org/10.1016/j.ajogmf.2019.100041
da Silva Lopes, K., Yamaji, N., Rahman, M. O., Suto, M., Takemoto, Y., Garcia-Casal, M. N., & Ota, E. (2021). Nutrition-specific interventions for preventing and controlling anaemia throughout the life cycle: an overview of systematic reviews. Cochrane Database of Systematic Reviews, 2021(9). https://doi.org/10.1002/14651858.CD013092.pub2
Dow, M. L., & Szymanski, L. M. (2020). Effects of Overweight and Obesity in Pregnancy on Health of the Offspring. Endocrinology and Metabolism Clinics of North America, 49(2), 251–263. https://doi.org/10.1016/j.ecl.2020.02.005
Forty, J., Rakgoasi, S. D., & Keetile, M. (2021). Patterns and determinants of modern contraceptive use and intention to usecontraceptives among Malawian women of reproductive ages (15–49 years). Contraception and reproductive medicine, 6, 1-12. https://doi.org/10.1186/s40834-021-00163-8
Frick, A. P. (2021). Advanced maternal age and adverse pregnancy outcomes. Best Practice and Research: Clinical Obstetrics and Gynaecology, 70(5), 92–100. https://doi.org/10.1016/j.bpobgyn.2020.07.005
Girma, A., Bedada, A., & Kumbi, S. (2023). Utilization of preconception care and associated factors among pregnant women attending ANC in private MCH Hospitals in Addis Ababa, Ethiopia. BMC Pregnancy and Childbirth, 23(1), 1–12. https://doi.org/10.1186/s12884-023-05955-1
Gul, R., Iqbal, S., Anwar, Z., Ahdi, S. G., Ali, S. H., & Pirzada, S. (2020). Pre-pregnancy maternal BMI as predictor of neonatal birth weight. PLoS ONE, 15(10 October), 1–9. https://doi.org/10.1371/journal.pone.0240748
Hamadneh, S., & Hamadneh, J. (2021). Active and passive maternal smoking during pregnancy and birth outcomes: A study from a developing country. Annals of Global Health, 87(1), 1–8. https://doi.org/10.5334/aogh.3384
Kim, H. Y., Cho, G. J., Ahn, K. H., Hong, S. C., Oh, M. J., & Kim, H. J. (2024). Short-term neonatal and long-term neurodevelopmental outcome of children born term low birth weight. Scientific Reports, 14(1), 2274. https://doi.org/10.1038/s41598-024-52154-9
Li, C., Zhu, N., Zeng, L., Dang, S., Zhou, J., Pei, L., Watson, V., Chen, T., Wang, D., & Yan, H. (2018). Effect of maternal pre-pregnancy underweight and average gestational weight gain on physical growth and intellectual development of early school-aged children. Scientific Reports, 8(1). https://doi.org/10.1038/s41598-018-30514-6
Li, N., Zhao, G., Wu, W., Zhang, M., Liu, W., Chen, Q., & Wang, X. (2020). The efficacy and safety of vitamin C for iron supplementation in adult patients with iron deficiency anemia: a randomized clinical trial. JAMA network open, 3(11), e2023644-e2023644. . https://doi.org/10.1001/jamanetworkopen.2020.23644
Mathewson, K. J., Burack, J. A., Saigal, S., & Schmidt, L. A. (2021). Tiny babies grow up: The long-term effects of extremely low birth weight. Prenatal stress and child development, 469-490. https://doi.org/10.1007/978-3-030-60159-1_16
Means, R. T. (2020). Iron deficiency and iron deficiency anemia: Implications and impact in pregnancy, fetal development, and early childhood parameters. Nutrients, 12(2). https://doi.org/10.3390/nu12020447
Ministry of Health RI. (2018). Buletin Stunting. Kementerian Kesehatan RI, 301(5), 1163–1178.
Ministry of Health RI. (2023). Indonesian basic health research 2023. Balitbang Kemenkes RI.
Mog, M., & Ghosh, K. (2021). Prevalence of anaemia among women of reproductive age (15–49): A spatial-temporal comprehensive study of Maharashtra districts. Clinical Epidemiology and Global Health, 11, 100712. https://doi.org/10.1016/j.cegh.2021.100712
Moradinazar, M., Najafi, F., Nazar, Z. M., Hamzeh, B., Pasdar, Y., & Shakiba, E. (2020). Lifetime prevalence of abortion and risk factors in women: evidence from a cohort study. Journal of pregnancy, 2020(1), 4871494. https://doi.org/10.1155/2020/4871494
Parmar, M. P., Kaur, M., Bhavanam, S., Mulaka, G. S. R., Ishfaq, L., Vempati, R., & Davalgi, S. (2023). A systematic review of the effects of smoking on the cardiovascular system and general health. Cureus, 15(4). https://doi.org/10.7759%2Fcureus.38073
Sainafat, A., Asmawati, Ikhlasiah, M., Mat, S. B., & Hassan, H. C. (2020). Preconception care in adolescents. Enfermeria Clinica, 30(2019), 73–76. https://doi.org/10.1016/j.enfcli.2019.11.024
Schüssler, S. C., Schmidt, M., Deiters, L., Candova, A., Fahlbusch, F. B., & Trollmann, R. (2022). Long-term outcomes of very-low-birth-weight and low-birth-weight preterm newborns with neonatal seizures: a single-center perspective. European Journal of Paediatric Neurology, 36, 137-142. https://doi.org/10.1016/j.ejpn.2021.12.013
Seshadri, S., Morris, G., Serhal, P., & Saab, W. (2021). Assisted conception in women of advanced maternal age. Best Practice & Research Clinical Obstetrics & Gynaecology, 70, 10-20. https://doi.org/10.1016/j.bpobgyn.2020.06.012
Shan, D., Qiu, P.-Y., Wu, Y.-X., Chen, Q., Li, A.-L., Ramadoss, S., Wang, R.-R., & Hu, Y.-Y. (2018). Pregnancy Outcomes in Women of Advanced Maternal Age: a Retrospective Cohort Study from China. Scientific Reports, 8(1). https://doi.org/10.1038/s41598-018-29889-3
Stephenson, J., Heslehurst, N., Hall, J., Schoenaker, D. A. J. M., Huchinson, J., Cade, J., Poston, L., Barrett, G., Crozier, S., Kumaran, K., Yanjik, C., Barker, M., Baird, J., & Mishra, G. (2018). Before the beginning: nutrition and lifestyle in the preconception period and its importance for future health. Lancet, 391(10132), 1830–1841. https://doi.org/10.1016/S0140-6736(18)30311-8
Toivonen, K. I., Oinonen, K. A., & Duchene, K. M. (2017). Preconception health behaviours. Preventive Medicine, 96(1), 1–15. https://doi.org/10.1016/j.ypmed.2016.11.022
UNICEF. (2022). Child Marriage Lastest Trends and Future Prospects. https://doi.org/10.1177/104438942500600710
World Health Organization (2022). GATS (Global Adult Tobacco Survey) Comparison Fact Sheet comparison Indonesia 2011 & 2021. https://cdn.who.int/media/docs/default-source/ncds/ncd-surveillance/data-reporting/indonesia/indonesia-national-2021----2011-comparison-factsheet.pdf?sfvrsn=46869411_1
Copyright (c) 2024 Nadya Dina Tazkiyah, Suprapti Suprapti, Lisa Purbawaning Wulandari, Sunaeni Sunaeni, Herawati Mansur

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
Authors retain copyright and grant the journal right of first publication with the work simultaneously licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License that allows others to share the work with an acknowledgment of the work's authorship and initial publication in this journal.
Authors are able to enter into separate, additional contractual arrangements for the non-exclusive distribution of the journal's published version of the work (e.g., post it to an institutional repository or publish it in a book), with an acknowledgment of its initial publication in this journal.
Authors are permitted to publish their work online in third parties as it can lead to wider dissemination of the work.






