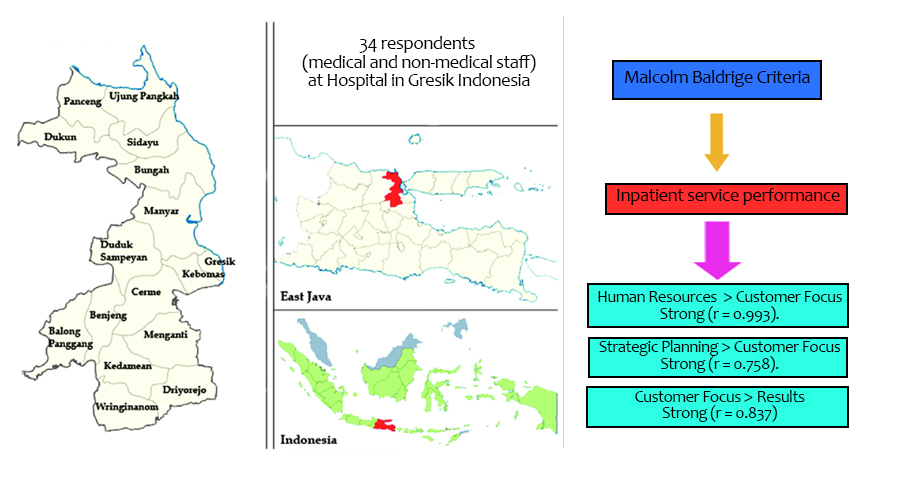
Improving Inpatient Unit Performance Through the Malcolm Baldrige Framework: A Study in a Hospital in Gresik, Indonesia
Abstract
Numerous studies have explored various aspects of performance in healthcare services, including patient satisfaction, staff well-being, and resource capacity. However, research addressing these gaps using the Malcolm Baldrige Performance Criteria framework remains limited. This study aims to evaluate and enhance the inpatient service performance at Mabarrot Gresik Islamic Hospital using the Malcolm Baldrige Performance Criteria model. An analytical observational study with a cross-sectional approach was conducted to analyze the relationships and correlations among eight Malcolm Baldrige criteria: Organizational Profile, Leadership, Strategic Planning, Customer Focus, Measurement, Analysis, and Knowledge Management, Human Resources, Operational Activity Focus, and Results. Data were collected from 34 respondents, comprising medical and non-medical staff, using a validated (CVI = 0.77) and reliable (α = 0.986) questionnaire. The analysis revealed that Human Resources (r = 0.993), Results (r = 0.837), and Strategic Planning (r = 0.758) demonstrated very strong relationships with Customer Focus, indicating these areas significantly impact inpatient service performance. Furthermore, a strong correlation was found between Customer Focus and Results (r = 0.837), emphasizing the importance of prioritizing patient satisfaction to achieve better outcomes. However, the study identified a weak relationship between the Organizational Profile and Measurement, Analysis, and Knowledge Management criteria, indicating a misalignment that requires attention. The findings suggest that improving human resource performance and addressing customer needs are critical strategies for enhancing inpatient services.
Downloads
References
Alibrandi, A., Gitto, L., Limosani, M., & Mustica, P. F. (2023). Patient satisfaction and quality of hospital care. Evaluation and Program Planning, 97, 102251. https://doi.org/10.1016/j.evalprogplan.2023.102251
Alkhaldi, R. Z., & Abdallah, A. B. (2020). Lean management and operational performance in health care: Implications for business performance in private hospitals. International Journal of Productivity and Performance Management, 69(1), 1-21. https://doi.org/10.1108/ijppm-09-2018-0342
Amorim-Lopes, M., Oliveira, M., Raposo, M., Cardoso-Grilo, T., Alvarenga, A., Barbas, M., & Barbosa-Póvoa, A. (2021). Enhancing optimization planning models for health human resources management with foresight. Omega, 103, 102384. https://doi.org/10.1016/j.omega.2020.102384
Baashar, Y., Alhussian, H., Patel, A., Alkawsi, G., Alzahrani, A. I., Alfarraj, O., & Hayder, G. (2020). Customer relationship management systems (CRMS) in the healthcare environment: A systematic literature review. Computer Standards & Interfaces, 71, 103442. https://doi.org/10.1016/j.csi.2020.103442
Bakhtiari, S., Sharif, F., Shahriari, M., & Rakhshan, M. (2020). Perspective and experience of hospital operating room nurses with the concept of excellence: A qualitative study. Risk management and healthcare policy, 125-134. https://doi.org/10.2147/RMHP.S236389
Bhati, D., Deogade, M. S., & Kanyal, D. (2023). Improving patient outcomes through effective hospital administration: a comprehensive review. Cureus, 15(10). https://doi.org/10.7759/cureus.47731
Bosque-Mercader, L., & Siciliani, L. (2023). The association between bed occupancy rates and hospital quality in the English National Health Service. The European Journal of Health Economics, 24(2), 209-236. https://doi.org/10.1007/s10198-022-01464-8
Dartanto, T., Pramono, W., Lumbanraja, A. U., Siregar, C. H., Bintara, H., & Sholihah, N. K. (2020). Enrolment of informal sector workers in the National Health Insurance System in Indonesia: A qualitative study. Heliyon, 6(11). https://doi.org/10.1016/j.heliyon.2020.e05316
Dion, H., & Evans, M. (2024). Strategic frameworks for sustainability and corporate governance in healthcare facilities; approaches to energy-efficient hospital management. Benchmarking: An International Journal, 31(2), 353-390. https://doi.org/10.1108/bij-04-2022-0219
Ekiz Kavukoğlu, T., & İşci, E. (2024). The mediating role of strategic planning awareness in the impact of organizational innovation on business excellence in hospitals. The TQM Journal, 36(8), 2527-2550. https://doi.org/10.1108/tqm-05-2023-0155
El-Gazar, H. E., & Zoromba, M. A. (2021). Nursing human resource practices and hospitals’ performance excellence: the mediating role of nurses’ performance. Acta Bio Medica: Atenei Parmensis, 92(Suppl 2). https://doi.org/10.23750/abm.v92iS2.11247
Hannawa, A. F., Wu, A. W., Kolyada, A., Potemkina, A., & Donaldson, L. J. (2022). The aspects of healthcare quality that are important to health professionals and patients: A qualitative study. Patient education and counseling, 105(6), 1561-1570. https://doi.org/10.1016/j.pec.2021.10.016
Hogan, D. R., Stevens, G. A., Hosseinpoor, A. R., & Boerma, T. (2018). Monitoring universal health coverage within the Sustainable Development Goals: development and baseline data for an index of essential health services. The Lancet Global Health, 6(2), e152-e168. https://doi.org/10.1016/s2214-109x(17)30472-2
KhanMohammadi, E., Talaie, H., & Azizi, M. (2023). A healthcare service quality assessment model using a fuzzy best–worst method with application to hospitals with in-patient services. Healthcare Analytics, 4, 100241. https://doi.org/10.1016/j.health.2023.100241
Lee, J. Y., McFadden, K. L., Lee, M. K., & Gowen III, C. R. (2021). US hospital culture profiles for better performance in patient safety, patient satisfaction, Six Sigma, and lean implementation. International Journal of Production Economics, 234, 108047. https://doi.org/10.1016/j.ijpe.2021.108047
Manzoor, F., Wei, L., Hussain, A., Asif, M., & Shah, S. I. A. (2019). Patient satisfaction with health care services; an application of physician’s behavior as a moderator. International journal of environmental research and public health, 16(18), 3318. https://doi.org/10.3390/ijerph16183318
Moinzad, H., & Akbarzadeh, M. H. (2022). How to improve information technology strategic planning effectiveness using balanced scorecard, risk and maturity analysis, case study health information technology? A qualitative study. Health Science Reports, 5(6), e926. https://doi.org/10.1002/hsr2.926
Niazi, M., Dehkordi, M. R., Eghbali, M., & Samadian, D. (2021). Seismic resilience index evaluation for healthcare facilities: A case study of hospital in Tehran. International Journal of Disaster Risk Reduction, 65, 102639.
Nurmeksela, A., Zedreck Gonzalez, J. F., Kinnunen, J., & Kvist, T. (2021). Components of the Magnet® model provide structure for the future vision of nurse managers’ work: A qualitative perspective of nurse managers. Journal of nursing management, 29(7), 2028-2036. https://doi.org/10.1111/jonm.13337
Olayiwola, R. K., Tuomi, V., Strid, J., & Nahan-Suomela, R. (2024). Impact of Total quality management on cleaning companies in Finland: A Focus on organisational performance and customer satisfaction. Cleaner Logistics and Supply Chain, 10, 100139. https://doi.org/10.1016/j.clscn.2024.100139
Ordu, M., Demir, E., Tofallis, C., & Gunal, M. M. (2023). A comprehensive and integrated hospital decision support system for efficient and effective healthcare services delivery using discrete event simulation. Healthcare Analytics, 4, 100248. https://doi.org/10.1016/j.health.2023.100248
Pishnamazzadeh, M., Sepehri, M. M., & Ostadi, B. (2020). An assessment model for hospital resilience according to the simultaneous consideration of key performance indicators: A system dynamics approach. Perioperative Care and Operating Room Management, 20, 100118.
Purba, H. H. (2021). A systematic literature review of Malcolm Baldrige national quality award (MBNQA). Journal of Technology Management for Growing Economies, 12(1), 1-12. https://doi.org/10.15415/jtmge.2021.121001
Rangsungnoen, G., Sroypetch, S., & Caldicott, R. W. (2024). Extending the Baldrige excellence model for managing community-based social enterprise. Social Enterprise Journal, 20(1), 1-31. https://doi.org/10.1108/SEJ-01-2023-0001
Rochmatullah, M. R., Rahmawati, R., Probohudono, A. N., & Widarjo, W. (2023). Is quantifying performance excellence really profitable? An empirical study of the deployment of the Baldrige Excellence Measurement Model in Indonesia. Asia Pacific Management Review, 28(3), 287-298. https://doi.org/10.1016/j.apmrv.2022.10.006
Saeidi, P., Robles, L. A. A., Saeidi, S. P., & Zamora, M. I. V. (2021). How does organizational leadership contribute to the firm performance through social responsibility strategies?. Heliyon, 7(7). https://doi.org/10.1016/j.heliyon.2021.e07672
Shanafelt, T., Stolz, S., Springer, J., Murphy, D., Bohman, B., & Trockel, M. (2020). A blueprint for organizational strategies to promote the well-being of health care professionals. NEJM Catalyst Innovations in Care Delivery, 1(6). https://doi.org/10.1056/CAT.20.0266
Suhail, P., & Srinivasulu, Y. (2021). Perception of service quality, satisfaction, and behavioral intentions in Ayurveda healthcare. Journal of Ayurveda and integrative Medicine, 12(1), 93-101. https://doi.org/10.1016/j.jaim.2020.10.011
Suriyankietkaew, S., & Kungwanpongpun, P. (2022). Strategic leadership and management factors driving sustainability in health-care organizations in Thailand. Journal of Health Organization and Management, 36(4), 448-468. https://doi.org/10.1108/JHOM-05-2021-0165
Tushar, S. R., Moktadir, M. A., Kusi-Sarpong, S., & Ren, J. (2023). Driving sustainable healthcare service management in the hospital sector. Journal of Cleaner Production, 420, 138310. https://doi.org/10.1016/j.jclepro.2023.138310
van Diggele, C., Burgess, A., Roberts, C., & Mellis, C. (2020). Leadership in healthcare education. BMC medical education, 20, 1-6. https://doi.org/10.1186/s12909-020-02288-x
Vanichchinchai, A. (2023). Relationships between leadership and culture, human resources and process improvement in lean healthcare. Business Process Management Journal, 29(2), 430-446. https://doi.org/10.1108/BPMJ-07-2022-0328
Wackers, E., Stadhouders, N., Heil, A., Westert, G., van Dulmen, S., & Jeurissen, P. (2021). Hospitals bending the cost curve with increased quality: a scoping review into integrated hospital strategies. International Journal of Health Policy and Management, 11(11), 2381. https://doi.org/10.34172/ijhpm.2021.168
Wang, Y., Peng, X., & Prybutok, V. (2022). The importance of information technology to organizational results within the Baldrige award. Quality Management Journal, 29(1), 3-17. https://doi.org/10.1080/10686967.2021.2006584
Weston, M. J. (2022). Strategic planning for a very different nursing workforce. Nurse leader, 20(2), 152-160. https://doi.org/10.1016/j.mnl.2021.12.021
Copyright (c) 2024 Setya Haksama, Diansanto Prayoga, Muhammad Azhary, Syahprevi Rayyan Zeinsar, Shyamkumar Sriram, Abdullah Al Mamun

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
Authors retain copyright and grant the journal right of first publication with the work simultaneously licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License that allows others to share the work with an acknowledgment of the work's authorship and initial publication in this journal.
Authors are able to enter into separate, additional contractual arrangements for the non-exclusive distribution of the journal's published version of the work (e.g., post it to an institutional repository or publish it in a book), with an acknowledgment of its initial publication in this journal.
Authors are permitted to publish their work online in third parties as it can lead to wider dissemination of the work.






